Durch Ashley Ridout, Osteopath, Functional Rehab Specialist & Pain Educator | Published on August 27, 2025

Wenn Sie Ihre Haltung “fixiert” haben — aber der Schmerz nicht aufhört
Du hast alles getan.
Ihr Monitor befindet sich auf Augenhöhe.
Ihr Stuhl verfügt über eine Lendenwirbelstütze.
Ihr Schreibtisch ist ergonomisch perfekt.
Sie sitzen aufrecht, die Schultern nach hinten, das Kinn eingezogen — genau wie die Experten sagen.
Und trotzdem … schmerzt Ihr Rücken immer noch.
Am Nachmittag verspannt sich Ihr Nacken immer noch.
An manchen Tagen beginnen die Schmerzen, bevor Sie sich überhaupt hinsetzen.
Wenn Ihnen das bekannt vorkommt, sind Sie nicht allein. Seit Jahrzehnten wird eine schlechte Körperhaltung für alles verantwortlich gemacht, von Rückenschmerzen bis hin zu Kopfschmerzen.
Aber hier ist die überraschende Wahrheit: Haltung allein ist selten die Ursache.
Tatsächlich leben viele Menschen mit einer sogenannten “perfekten” Haltung mit Schmerzen, während viele Menschen mit einer “unvollkommenen” Haltung schmerzfrei sind.
Untersuchungen zeigen immer wieder, dass die Körperhaltung ein schwacher —und manchmal nicht vorhandener — Prädiktor für chronische Schmerzen ist.
Also, was ist los?
Warum leiden manche Menschen trotz “korrigierender” Haltung immer wieder unter Schmerzen?
Was ich in der Klinik sehe (14+ Jahre, Tausende von Fällen)

ich war ein Osteopathen Seit über 14 Jahren hilft es allen, vom Schreibtischprofi bis zum Spitzensportler, sich von Verletzungen zu erholen, wieder funktionsfähig zu sein und ohne Schmerzen zu leben. Meine Arbeit vermischt:
- manueller Therapie
- Functional Rehab
- Trainingsprogramm
- Ausbildung in Schmerzneurowissenschaften
- Gegebenenfalls funktionelle Medizin und ergänzende Therapien
In dieser Zeit habe ich mit Menschen gearbeitet, die sich von Kreuzbandrekonstruktionen, gefrorenen Schultern, chronischen Kopfschmerzen, Verletzungen durch wiederholte Belastung und jahrelangen Wirbelsäulenschmerzen erholten.
In all diesen Fällen zeigt sich immer wieder ein Muster: Menschen Fixieren Sie ihre Haltung Aber immer noch verletzt —, weil das Problem nicht darin besteht, wie sie sitzen, stehen oder heben.
Das Problem ist, wie ihre Das Nervensystem reguliert den Muskeltonus.
Wenn du alles richtig machst — aber immer noch Schmerzen hast
Einige meiner Patienten kommen mit einer tadellosen Körperhaltung und einer für sie typischen ergonomischen Ausstattung an.
Sie dehnen sich, sie stärken sich, sie machen ihre vorgeschriebenen Übungen.
Und trotzdem:
- Ihre Muskeln fühlen sich “verspannt” an, bevor sie überhaupt in den Tag starten.
- Auf der Suche nach Komfort wechseln sie alle paar Minuten ihren Stuhl.
- Even light activity leaves their back feeling strained.
Das ist keine Faulheit.
Es ist nicht “schlechte Form.”
Es geht nicht darum, den Plan zu ignorieren. Es ist ein Nervensystem, das in einem Muster feststeckt Übermäßiger Schutz des Körpers.

Haltung vs. Muskeltonus — Der Unterschied, der die Behandlung verändert
Körperhaltung ist die sichtbare Position Ihres Körpers.
Ton ist die unsichtbare Bereitschaft Ihrer Muskeln, sich zusammenzuziehen.
Befindet sich das Nervensystem in einem längeren Zustand “Kampf oder Flucht”, bleibt der Tonus erhöht — auch im Ruhezustand.
Diese ständige Kontraktion auf niedrigem Niveau komprimiert die Gelenke, schränkt den Blutfluss ein und sensibilisiert die Nerven.
Es ist, als würde man den ganzen Tag leicht mit den Schultern zucken, ohne es zu merken.
Mit der Zeit entsteht dadurch genau das Unbehagen, für das die Leute verantwortlich sind “schlechte Körperhaltung”
Die Rolle des Nervensystems bei Muskelverspannungen
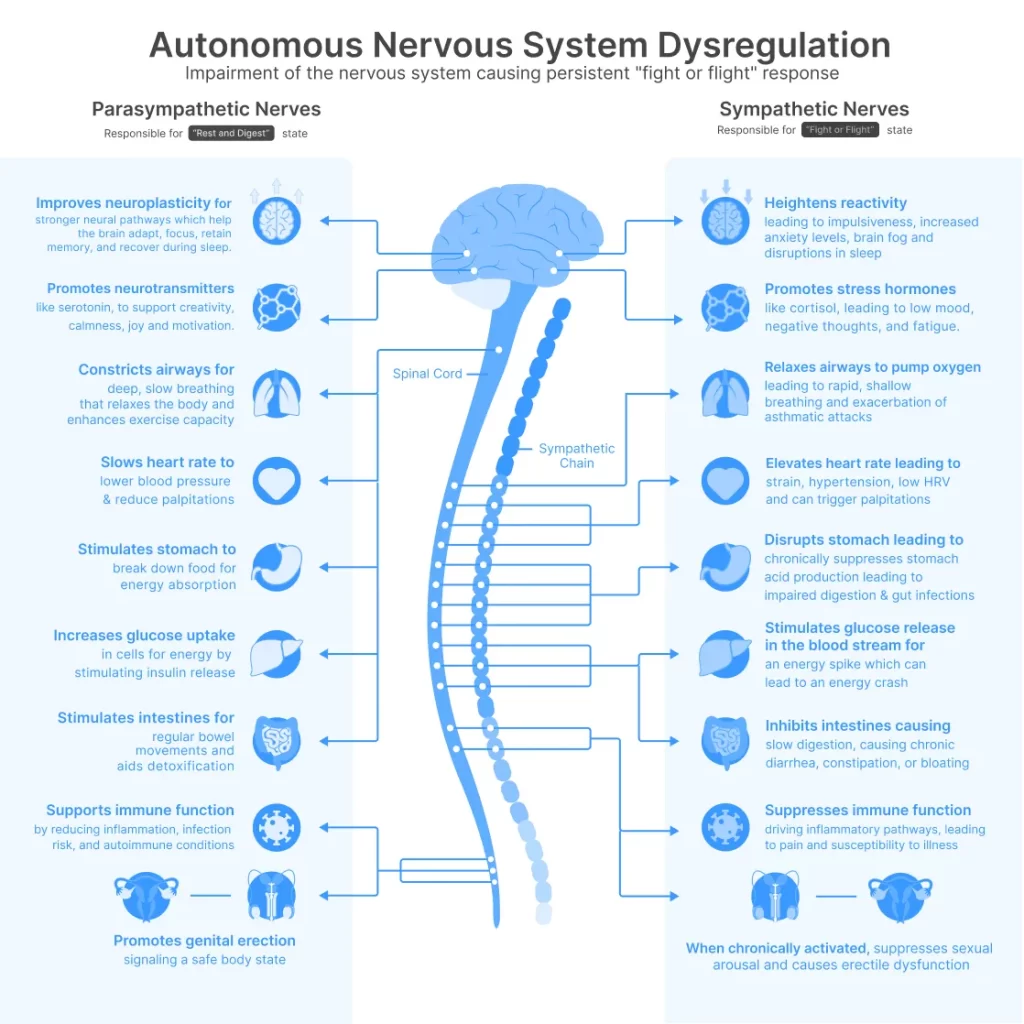
Die autonomes Nervensystem hat zwei Hauptmodi:
- sympathisch (“Kampf oder Flucht”) — einsatzbereit
- Parasympathisch (“ausruhen, verdauen, reparieren”) — bereit zur Erholung
In einem idealen System bewegen Sie sich reibungslos zwischen beiden. Aber Stress — körperlich, geistig, emotional — kann das Gleichgewicht in Richtung einer ständigen sympathischen Aktivierung verschieben.
Das bedeutet, dass Ihr Körper Spannung hält nur für den Fall, auch wenn du vollkommen still bist.
Und wenn Ihr Gehirn eine Bedrohung wahrnimmt (auch unbewusst), kann es diese Muskeln auf unbestimmte Zeit “auf der Hut” halten.
Der Vagusnerv: Ihr Ruheschalter
Eine der wichtigsten Kontrolllinien für parasympathische Aktivität ist die Vagusnerv — ein langer Hirnnerv, der von Ihrem Hirnstamm durch Ihre Brust und Ihren Bauch verläuft.
als Vagustonus ist stark, Ihr Körper kann leicht in den Erholungsmodus wechseln, die Muskeln können sich entspannen und die Schmerzempfindlichkeit kann abnehmen.
Wenn es schwach ist, bleibt Ihr System auf Gefahren vorbereitet — die Anspannung bleibt bestehen, der Schlaf leidet und kleine Reizungen können große Schübe auslösen.
Was die Forschung sagt
Die Wissenschaft bestätigt, was ich in der Klinik sehe:
- Die Körperhaltung allein ist kein zuverlässiger Prädiktor für Schmerzen — Groß angelegte Untersuchungen zeigen keinen konsistenten kausalen Zusammenhang zwischen Körperhaltung und chronischen Rückenschmerzen.¹ ²
- taVNS (transkutane Stimulation des Nervus auricularis vagus) — Derselbe Ansatz, der in Nurosym — verwendet wird, hat sich als: erwiesen
- steigern HRV (Herzfrequenzvariabilität), ein Marker für eine ausgeglichene Aktivität des Nervensystems³
- Reduzieren Sie entzündliche Zytokine wie IL-6 und TNFalpha⁴ ⁵
- Verbessern Sie die konditionierte Schmerzmodulation —das integrierte Schmerzkontrollsystem des Körpers⁶
- Reduzieren Sie den Ruhemuskeltonus in den Zielmuskelgruppen⁷
- steigern HRV (Herzfrequenzvariabilität), ein Marker für eine ausgeglichene Aktivität des Nervensystems³
- Sicherheit: Über 50 veröffentlichte Studien, darunter Kooperationen mit Harvard, Yale und dem Imperial College London, haben berichtet keine schweren Nebenwirkungen wenn taVNS richtig verwendet wird.⁸
Wo Nurosym zum Einsatz kommt (Unterstützung zu Hause)

In meiner Praxis beschäftige ich mich sowohl mit Mechanik (Gelenkbeweglichkeit, Gewebegesundheit, Bewegungsmuster) als auch mit Neurobiologie (Empfindlichkeit, Tonus, Erholung).
Für einige Patienten — insbesondere solche mit anhaltendem Muskelschutz trotz guter Reha — schlage ich ein Instrument zur Unterstützung des Nervensystems zu Hause vor.
hier Nurosym ins Spiel.
- Was es ist: Ein CE-gekennzeichnetes taVNS-Gerät, das an einem Teil des Ohrs befestigt wird, der mit dem Vagusnerv verbunden ist.
- So funktioniert es: Liefert sanfte elektrische Impulse, um die parasympathische Aktivität zu stimulieren.
- Warum ich es empfehle: Um zu helfen “die Zuwächse zu halten”, die wir während der Sitzung erzielen, insbesondere zwischen den Behandlungen oder während Phasen mit hohem Stress.
ist es nicht Ein Allheilmittel oder ein Ersatz für praktische Pflege. Aber für den richtigen Patienten kann es einen zusätzlichen Anstoß zur Genesung geben — und dem Nervensystem helfen, unnötige Spannungen loszulassen.
reale Anwendungsfälle
- Der High-Stress-Profi — Sie können die Arbeitsbelastung nicht reduzieren, müssen aber aufhören, sie auf ihren Schultern zu tragen.
- Der Patient nach der Verletzung — Frei für Bewegung, aber das Nervensystem bewacht immer noch den verletzten Bereich.
- Der Fall “Ich habe alles versucht” — Ergonomie, Physiotherapie, Dehnen erledigt; Spannung immer noch da.
- Der schlaflose, schmerzende Rücken — Schmerzen, die nachts oder beim Aufwachen schlimmer sind und mit einer Überaktivität des Nervensystems zusammenhängen.
Wer könnte davon profitieren — und wer sollte es nicht nutzen
Könnte profitieren:
- Büroangestellte mit anhaltender Nacken-/Rückenverspannung
- Personen mit “unerklärlichen” Haltungsschmerzen trotz guter Ausrichtung
- Reha-Patienten, deren Muskeltonus trotz körperlicher Betätigung hoch bleibt
- Menschen mit schlechtem Schlaf und hohem Stress tragen zur Morgensteifheit bei
Vermeiden Sie es, wenn:
- Sie verfügen über einen Herzschrittmacher oder ein implantierbares Herzgerät
- du schwanger bist
- Sie hatten kürzlich ein schweres Herzereignis
- Du bist unter 18
Befolgen Sie vor Beginn immer den ärztlichen Rat.
Eine sichere Möglichkeit, es auszuprobieren
- 30-Tage-Geld-zurück-Garantie — Erkunden Sie zu Hause ohne Risiko.
- Begrenzte Studienplätze verfügbar — Einige Teilnehmer erhalten möglicherweise einen Zuschuss von ~€70 als Gegenleistung für die Bereitstellung von Feedback.
Ich helfe Patienten bei der Entscheidung, ob dies gut passt, richte das Gerät richtig ein und integriere es in einen umfassenderen Genesungsplan.

Abschließende Gedanken: Behandeln Sie das System, nicht den Slouch
Wenn Sie “perfekte Haltung” ohne Erleichterung verfolgt haben, ist es vielleicht an der Zeit, tiefer zu schauen. Die Position Ihres Körpers ist wichtig — aber die staatlich Ihres Nervensystems ist oft wichtiger.
Durch die Beruhigung des Systems, das den Muskeltonus steuert, können Sie Ihre Haltung endlich natürlich und nicht erzwungen anfühlen — und sich ohne ständige Beschwerden bewegen.
Durch die Beruhigung des Systems, das den Muskeltonus steuert, können Sie Ihre Haltung endlich natürlich und nicht erzwungen anfühlen — und sich ohne ständige Beschwerden bewegen.
Referenzen
- Back to basics: 10 facts every person should know about back pain. O’Sullivan, P. B., Caneiro, J. P., O’Sullivan, K., Lin, I., Bunzli, S., Wernli, K., & O’Keeffe, M. (2020). British Journal of Sports Medicine, 54(12), 698–699. https://doi.org/10.1136/bjsports-2019-101611
- No consensus on causality of spine postures or physical exposure and low back pain: A systematic review of systematic reviews. Swain, C. T. V., Pan, F., Owen, P. J., Schmidt, H., & Belavy, D. L. (2020). Journal of Biomechanics, 102, 109312. https://doi.org/10.1016/j.jbiomech.2019.08.006
- Does transcutaneous auricular vagus nerve stimulation affect vagally mediated heart rate variability? A living and interactive Bayesian meta-analysis. Wolf, V., Kühnel, A., Teckentrup, V., Koenig, J., & Kroemer, N. B. (2021). Psychophysiology, 58(11), e13933. https://doi.org/10.1111/psyp.13933
- Ear your heart: transcutaneous auricular vagus nerve stimulation on heart rate variability in healthy young participants. Forte, G., Favieri, F., Leemhuis, E., De Martino, M. L., Giannini, A. M., De Gennaro, L., Casagrande, M., & Pazzaglia, M. (2022). PeerJ, 10, e14447. https://doi.org/10.7717/peerj.14447
- Transcutaneous vagal nerve stimulation blocks stress-induced activation of interleukin-6 and interferon-γ in posttraumatic stress disorder: A double-blind, randomized, sham-controlled trial. Bremner, J. D., Gurel, N. Z., Jiao, Y., Wittbrodt, M. T., Levantsevych, O. M., Huang, M., Jung, H., Shandhi, M. H., Beckwith, J., Herring, I., Rapaport, M. H., Murrah, N., Driggers, E., Ko, Y.-A., Alkhalaf, M. L., Soudan, M., Song, J., Ku, B. S., Shallenberger, L., … Pearce, B. D. (2020). Brain, Behavior, & Immunity – Health, 9, 100138. https://doi.org/10.1016/j.bbih.2020.100138
- Transcutaneous auricular vagus nerve stimulation reduces cytokine production in sepsis: An open double-blind, sham-controlled, pilot study. Wu, Z., Zhang, X., Cai, T., Li, Y., Guo, X., Zhao, X., Wu, D., Li, Z., & Zhang, L. (2023). Brain Stimulation, 16(2), 507–514. https://doi.org/10.1016/j.brs.2023.02.008
- Transauricular vagus nerve stimulation (taVNS) enhances conditioned pain modulation (CPM) in healthy subjects: A randomized controlled trial. Pacheco-Barrios, K., Gianlorenço, A. C., Camargo, L., Andrade, M. F., Choi, H., Song, J. J., & Fregni, F. (2024). Brain Stimulation, 17(2), 346–348. https://doi.org/10.1016/j.brs.2024.03.006
- Transcutaneous auricular vagus nerve stimulation modulates masseter muscle activity, pain perception, and anxiety levels in university students: A double-blind, randomized, controlled clinical trial. Ferreira, L. M. A., Brites, R., Fraião, G., Pereira, G., Fernandes, H., de Brito, J. A. A., Pereira Generoso, L., Maziero Capello, M. G., Santos Pereira, G., Scoz, R. D., Silva, J. R. T., & Silva, M. L. (2024). Grenzen der integrativen Neurowissenschaft, 18, 1422312. https://doi.org/10.3389/fnint.2024.1422312
- Safety and tolerability of transcutaneous vagus nerve stimulation in humans: A systematic review. Redgrave, J., Day, D., Leung, H., Laud, P. J., Ali, A., Lindert, R., & Majid, A. (2018). Hirnstimulation, 11(6), 1225–1238. https://doi.org/10.1016/j.brs.2018.08.010
- Safety of transcutaneous auricular vagus nerve stimulation (taVNS): A systematic review and meta-analysis. Kim, A. Y., Marduy, A., de Melo, P. S., Gianlorenco, A. C., Kim, C. K., Choi, H., Song, J. J., & Fregni, F. (2022). Wissenschaftliche Berichte, 12(1), 22055. https://doi.org/10.1038/s41598-022-25864-1
- Parasym Device – Compliance and regulatory status. Parasym Ltd. (n.d.). Parasym Official Website. Retrieved August 18, 2025, from https://www.parasym.co/compliance.html
- Nurosym certification (CE Mark) information. Parasym Ltd. (2024, December 9). Nurosym Care Center – FAQ. Retrieved August 18, 2025, from https://care.nurosym.com/hc/en-us/articles/25945331731597-Is-Nurosym-a-certified-device
Der Artikel stellt in keiner Weise eine medizinische Beratung dar. Bitte konsultieren Sie einen zugelassenen Arzt, bevor Sie eine Behandlung beginnen. Diese Website kann Provisionen für die in diesem Artikel erwähnten Links oder Produkte erhalten.
Medically reviewed by Dr Anne Therese Bernadette Laudato, MD
Teilen über:



Finally someone says it’s not just “bad posture.” Been chasing perfect ergonomics for years.