Wichtige Punkte
- Der 3D-Druck ermöglicht hochgradig personalisierte Arzneimitteldosen auf‑Bedarf in Kliniken und Krankenhäusern.
- Von der FDA zugelassenes Beispiel: Spritam® (Levetiracetam), das Bindemittelstrahlen mit einer hochporösen Struktur zur schnellen Auflösung verwendet—hilfreich für Personen mit Schluckbeschwerden.
- Kernmethoden: Fused Deposition Modeling (FDM), Binder Jetting, Stereolithographie (SLA), Semi‑Solid Extrusion.
- Vorteile: maßgeschneiderte Dosierung, Multi‑Arzneimittel “Polypillen,” verbesserte Adhärenz, reduzierter Abfall.
- Einschränkungen: Produktionsgeschwindigkeit, Skalierbarkeit, Kosten, Qualitätskontrolle, sich entwickelnde Regulierung.
- Pilotprogramme und regulatorische Entwicklungen deuten auf eine transformative Zukunft im allgemeinen Gesundheitswesen hin.
Von Sci‑Fi zur Krankenhausrealität
Stellen Sie sich eine Krankenhausapotheke vor, in der irgendwann in der Zukunft ein Rezept in die Software eingegeben werden kann – und dann eine individuell dosierte Pille für den einzelnen Benutzer gedruckt wird, die auf sein Alter, Gewicht und seine Dosierungsbedürfnisse zugeschnitten ist. Keine Pillenaufteilung, komplizierten Zeitpläne oder vergessenen Dosen mehr. Dies ist kein ferner Traum – Spritam®, genehmigt von den USA. Die Food and Drug Administration (FDA) war 2015 das erste 3D‑-gedruckte Arzneimittel, das der Öffentlichkeit zugänglich war, und signalisierte damit, dass eine On‑Demand-Herstellung im Gesundheitswesen möglich ist.
Warum dies für das Gesundheitswesen wichtig ist
Die traditionelle Arzneimittelherstellung ist auf die Massenproduktion ausgelegt: Millionen identischer Pillen in festen Dosen. Obwohl dieses Modell effizient ist, lässt es wenig Raum für Personalisierung. Kinder, ältere Erwachsene und Anwender mit mehreren Rezepten haben oft Schwierigkeiten, Medikamente wie verschrieben einzunehmen – sei es aufgrund von Schluckbeschwerden, unbequemen Pillengrößen oder mangelnder Dosierungsflexibilität. Jüngsten Untersuchungen zufolge bietet der 3D-Druck eine Lösung, indem er eine individuelle Dosisanpassung ermöglicht und sogar mehrere Medikamente in einer einzigen Tablette kombiniert.
Die aktuellen Schmerzpunkte in der Medizin
Für viele Anwender ist das Problem nicht der Zugang zu Medikamenten – es ist die richtige Einnahme. Tabletten mit fester Dosis entsprechen möglicherweise nicht für jeden Einzelnen der optimalen therapeutischen Dosis. Menschen mit Schluckbeschwerden stehen täglich vor einer Herausforderung und greifen manchmal auf zerdrückende Pillen zurück, was die Freisetzung und Wirksamkeit des Arzneimittels verändern kann. Polypharmazie – wenn mehrere Medikamente verschrieben werden – erschwert die Therapietreue zusätzlich und erhöht die Wahrscheinlichkeit vergessener oder falscher Dosen.
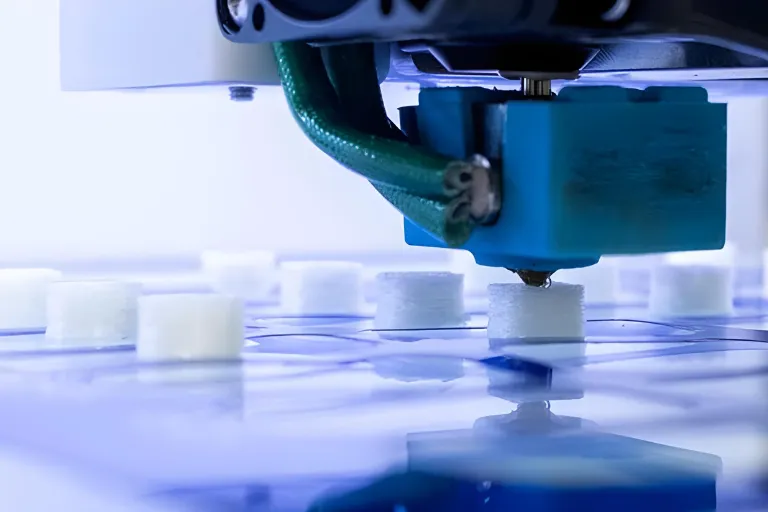
Wie 3D-Druck eine Pille erzeugt
Beim 3D-Druck in der Pharmaindustrie kommen mehrere Haupttechniken zum Einsatz:
- Binder Jetting – Ein wirkstoffhaltiges Pulver wird mit einem flüssigen Bindemittel Schicht für Schicht miteinander verbunden. Diese in Spritam® verwendete Methode erzeugt eine poröse Tablette, die sich schnell in kleinen Flüssigkeitsmengen auflöst.
- Fused Deposition Modeling (FDM) – Mit Arzneimitteln beladenes Polymerfilament wird unter Hitze extrudiert, was eine präzise Kontrolle über Dosis, Form und Arzneimittelfreisetzungsprofil ermöglicht.
- Stereolithographie (SLA) – Mit Arzneimittelmolekülen infundiertes lichtempfindliches Harz wird Schicht für Schicht mit einem Laser ausgehärtet, ideal für wärme‑empfindliche Verbindungen.
- Semi‑Solid Extrusion (SSE) – Pastenartige Formulierungen werden bei niedrigen Temperaturen extrudiert und eignen sich für unter Hitze instabile Arzneimittel.
Die Wahl der Methode hängt von der Stabilität des Arzneimittels, der gewünschten Freisetzungsrate und der Druckumgebung ab. Polymere, Hydrogele und Hilfsstoffe in pharmazeutischer Qualität werden sorgfältig ausgewählt, um Stabilität und vorhersehbare Arzneimittelfreisetzung zu gewährleisten.
Wo es bereits in Aktion ist
Über Spritam® hinaus haben Krankenhäuser in Spanien und Großbritannien den 3D-Druck für personalisierte Krebstherapietabletten und pädiatrische Formulierungen erprobt. Diese Projekte zeigten, dass die Point-of-Care-Produktion mit der Bioverfügbarkeit konventionell hergestellter Medikamente mithalten und gleichzeitig die Akzeptanz beim Anwender verbessern kann. Forschungslabore nutzen außerdem den 3D-Druck, um mehrere Medikamente “Polypillen” gegen Herz-Kreislauf-Erkrankungen herzustellen, indem sie mehrere Wirkstoffe in einer Tablette für den täglichen Gebrauch kombinieren.
Hürden bei Regulierung und Sicherheit
Während die Zulassung von Spritam® durch die FDA einen Präzedenzfall schuf, arbeiten die meisten Gesundheitsbehörden noch immer an detaillierten Richtlinien für 3D-gedruckte Medikamente, insbesondere für solche, die vor Ort in Krankenhäusern oder Apotheken hergestellt werden. Zu den regulatorischen Prioritäten gehören die Gewährleistung der Chargenkonsistenz, die Verhinderung gefälschter Produktion und die Festlegung von Schutzmaßnahmen für geistiges Eigentum. Auch die Europäische Arzneimittel-Agentur (EMA) evaluiert Rahmenwerke zur Integration des Point-of-Care-3D-Drucks in die regulierte Lieferkette.
Das Versprechen und die Fallstricke
| potenzielle Vorteile | derzeitigen Beschränkungen |
| Personalisierte Dosierung, abgestimmt auf die Bedürfnisse des Benutzers | Langsamere Produktion als Massenproduktion |
| Multi‑Medikament “Polypillen” zur Vereinfachung der Behandlungsschemata | Hohe Ausrüstungs- und Schulungskosten |
| Verbesserte Schluckfähigkeit und Adhärenz | Regulatorische Unsicherheit beim Point-of-Care-Druck |
| Weniger Abfall und besseres Bestandsmanagement | Bedarf an Spezialmaterialien und arzneimittelbeladenen Rohstoffen‑ |
Spotlight: Fallstudie zu Spritam®
Spritam® (Levetiracetam) verwendet das Bindemittel-®Jetting-Verfahren ZipDose‑ von Aprecia, um eine Tablette herzustellen, die sich mit einem Schluck Flüssigkeit in Sekundenschnelle auflöst. Es wurde für Menschen mit Schluckbeschwerden entwickelt, bietet eine präzise Dosierung und entspricht der Bioverfügbarkeit herkömmlicher Formen. Seine Zulassung zeigte, dass 3D-gedruckte Arzneimittel die Sicherheits-, Wirksamkeits- und Herstellungsqualitätsstandards erfüllen können.
Was kommt als Nächstes für 3D-gedruckte Medikamente
Die nächste Innovationswelle umfasst KI‑gesteuertes Tablet-Design zur Optimierung der Arzneimittelfreisetzung, biologisch abbaubare Implantate für eine nachhaltige Therapie und skalierte Krankenhausnetzwerke, die in der Lage sind, personalisierte Dosen im‑Haus herzustellen. Der Multi‑Drug-Druck könnte die Pillenbelastung bei der Behandlung chronischer Krankheiten verringern, während die Integration genomischer Daten ultra‑personalisierte Therapien ermöglichen könnte, die auf das Stoffwechselprofil einer Person zugeschnitten sind.
Ihre nächsten Schritte
Interessiert an der Zukunft der personalisierten Medizin? Fragen Sie Ihren Apotheker oder Gesundheitsdienstleister, wie neue 3D-Drucktechnologien eines Tages die Präzision und den Komfort der Behandlung verbessern können. Bleiben Sie auf dem Laufenden, indem Sie die regulatorischen Aktualisierungen der FDA und der EMA verfolgen, während sich dieser Bereich schnell weiterentwickelt.
Verantwortungsvoll voranschreiten
Für Angehörige der Gesundheitsberufe und Pharmaunternehmen liegt der Schlüssel darin, Innovation und Sicherheit in Einklang zu bringen. Krankenhäuser, die sich mit dem 3D-Druck befassen, benötigen robuste Qualitätskontrollsysteme, die Einhaltung gesetzlicher Vorschriften und geschultes Personal. Pharmazeutische Interessengruppen können in Partnerschaften, die die sichere Einführung beschleunigen, einen Wettbewerbsvorteil finden. Mit der Weiterentwicklung der Technologie könnte die Möglichkeit, personalisierte Medikamente auf Abruf herzustellen, die Art und Weise, wie Therapien bereitgestellt werden, grundlegend verändern – und uns einer präzisen Gesundheitsversorgung für alle näher bringen.
Dieser Blogbeitrag soll informativ sein und sollte keine professionelle Gesundheitsberatung ersetzen. Konsultieren Sie immer einen Arzt, um eine individuelle Beratung zu erhalten.
Referenzen
- Peng H, Han B, Tong T, Jin X, Peng Y, Guo M, et al. 3D printing processes in precise drug delivery for personalized medicine. Biofabrication. 2024 Apr 17;16(3):032001–1.
- Sutanto H. Tackling Polypharmacy in Geriatric Patients: Is Increasing Physicians’ Awareness Adequate? Archives of Gerontology and Geriatrics Plus. 2025 Jun;2(3):100185.
- Wang S, Chen X, Han X, Hong X, Li X, Zhang H, et al. A Review of 3D Printing Technology in Pharmaceutics: Technology and Applications, Now and Future. A Review of 3D Printing Technology in Pharmaceutics: Technology and Applications, Now and Future [Internet]. 2023 Jan 26;15(2):416–6. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9962448/
- Anaya BJ, Cerda JF, Datri R, Yuste I, Luciano FC, Kara A, et al. Engineering of 3D printed personalized polypills for the treatment of the metabolic syndrome. International Journal of Pharmaceutics. 2023 Jul 1;642:123194–4.



The idea of printing medicine to fit a person instead of forcing people to fit a pill sounds like the future.
If this helps people who struggle to swallow tablets, that alone makes it feel worth it.