Key Points
- Artificial Intelligence (AI) is redefining diagnostics and personalized therapy through tools like machine learning, computer vision, and natural language processing.
- AI-driven systems have improved diagnostic accuracy in fields like radiology, dermatology, cardiology, and oncology.
- Personalized therapy is becoming more adaptive and precise, thanks to AI-based drug discovery, genomics, and wearable technology.
- Integration of AI into healthcare raises ethical, regulatory, and logistical concerns, including bias, data privacy, and clinician trust.
- Real-world implementation shows both promise and resistance; the future of AI in medicine depends on human-AI collaboration and clear regulatory oversight.
A Revolution You Can’t Ignore
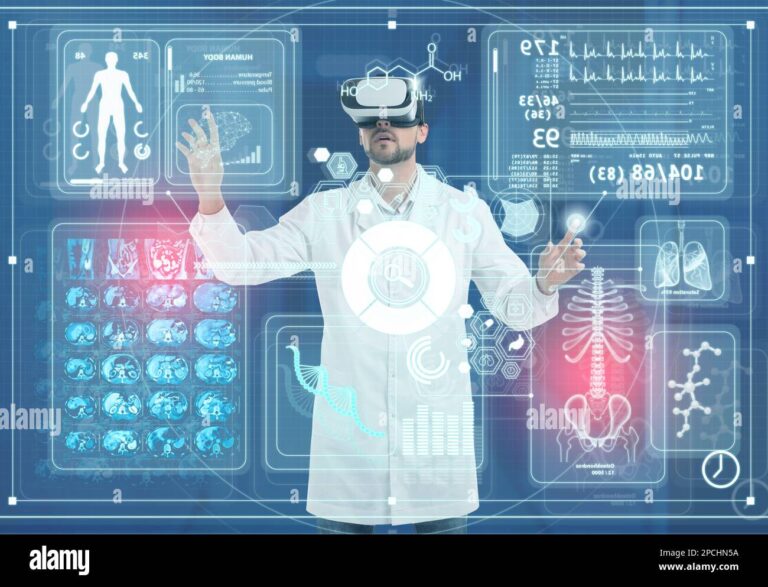
In 2016, Google’s DeepMind shocked the medical world when its AI system outperformed expert radiologists in detecting more than 50 eye conditions using retinal scans, achieving 94% accuracy in triaging urgent cases—often catching what human clinicians missed (De Fauw et al., 2018). Fast-forward to today, and AI isn’t just analyzing images. It’s predicting heart problems, detecting cancer earlier, and guiding therapy based on individual biology.
Artificial Intelligence in healthcare isn’t science fiction—it’s now a partner in diagnosis and decision-making. But with its promise comes critical questions: Can we trust algorithms with life-and-death calls? Who ensures these tools are fair and safe? This article explores how AI is reshaping healthcare—and what’s at stake if we get it wrong.
What Is AI in Healthcare, Really?
At its core, AI in healthcare refers to computer systems that simulate human intelligence to extract insights from medical data. These systems fall into categories like:
- Machine Learning (ML): Used to predict disease risk or outcomes by training on massive datasets (Jiang et al., 2017).
- Deep Learning: Especially useful for image interpretation, as in radiology and dermatology.
- Natural Language Processing (NLP): Used to mine insights from electronic medical records (EMRs), research papers, and clinician notes (Shickel et al., 2018).
- Computer Vision: Enables AI to interpret diagnostic images like X-rays or pathology slides.
These technologies have evolved from rule-based systems in the 1980s to today’s data-driven models, thanks to more accessible computing power and digitized medical data.
Diagnosing with More Precision Than Ever
AI is already outperforming humans in select diagnostic tasks. A 2020 study in Nature revealed that Google Health’s deep learning model reduced false positives by 5.7% and false negatives by 9.4% in breast cancer screenings compared to six expert radiologists (McKinney et al., 2020).
In emergency settings, platforms like Aidoc help health professionals flag pulmonary embolisms or strokes within minutes—cutting time-to-treatment and improving survival rates (Aidoc, 2023). Meanwhile, Tempus combines pathology, EMRs, and genomics to inform cancer therapy decisions, especially in complex cases.
Dermatology is also seeing transformation. AI models trained on thousands of skin lesion images can detect melanoma with accuracy comparable to or exceeding dermatologists, according to a 2020 Lancet Digital Health study (Tschandl et al., 2020).
From One-Size-Fits-All to Tailored Therapy
AI is revolutionizing the transition from reactive to proactive care:
- Drug Discovery: Companies like Insilico Medicine use AI to model how drugs interact with human biology, speeding up discovery while cutting R&D costs (Zhou et al., 2021).
- Genomics: DeepMind’s AlphaFold solved the decades-old challenge of predicting protein folding with near-lab accuracy, unlocking insights into inflammatory gut issues, autoimmune conditions, and cancer biology (Senior et al., 2020).
- Wearable Devices: Smart technologies now track biometrics and trigger interventions in real time. AI-driven vagal neuromodulation systems, for instance, are being explored to dynamically support mental balance, reduce trauma symptoms, and aid sleep problems (Fauver et al., 2021).
Personalized medicine guided by AI not only boosts effectiveness but also reduces side effects by accounting for user-specific genetics, comorbidities, and behavior.
Ethical, Clinical, and Regulatory Hurdles
Yet the AI revolution brings real challenges.
- Bias in Datasets: An AI tool widely used in U.S. hospitals was found to systematically underestimate the care needs of Black users by relying on historical healthcare spending instead of clinical data (Obermeyer et al., 2019).
- Explainability: Most AI models, especially deep neural networks, are considered “black boxes,” making it hard to explain their decisions—a barrier to clinical trust (Doshi-Velez & Kim, 2017).
- Privacy: Ensuring HIPAA and GDPR compliance is especially complex when AI tools access real-time data streams.
- Regulatory Oversight: The FDA has approved several AI-based tools, including IDx-DR for diabetic eye screening, under its Software as a Medical Device (SaMD) framework (FDA, 2020).
However, approval criteria vary globally. While the U.S. and EU are developing adaptive pathways for AI tools, most countries still lack robust regulatory blueprints.
Subscribe for Free for more insightful health articles tailored to your needs.
Are Health Professionals on Board?
It depends. In a 2023 Stanford Medicine report, 85% of health professionals said AI could help reduce documentation burdens, but only 38% trusted it for diagnostic decision-making (Stanford Medicine 2023 Health Trends Report).
The resistance often comes from concerns over workflow disruption, training needs, and liability. However, collaborative models, where AI supports—but does not override—clinical judgment, are gaining popularity. Institutions like Mayo Clinic and Cleveland Clinic are now co-designing AI solutions with physician input to ensure relevance and usability.
The Future: What’s Coming Next
What lies ahead?
- Generative AI tools like ChatGPT and Med-PaLM are being tested for documentation, decision support, and patient education (Singhal et al., 2022).
- Federated Learning allows AI models to be trained across decentralized data sources—minimizing privacy risks while improving accuracy.
- AI in Mental Health: Tools analyzing voice, text, or facial expressions may soon detect trauma, anxious thoughts, or depressive states before symptoms become visible (Guntuku et al., 2017).
But for all its promise, AI must prove its value not just in lab studies, but in real-world practice—amid diverse users, imperfect data, and time-pressed health professionals.
Where Do We Go From Here?
Artificial Intelligence holds the potential to enhance nearly every facet of modern medicine—but only when guided by transparency, equity, and ethics. Health professionals should seek tools that enhance—not overcomplicate—their workflow. Policy-makers must push for fair, explainable, and secure systems. And users deserve visibility into how algorithms influence their care.
To learn more about approved AI medical tools, visit the FDA’s SaMD listings or explore the World Health Organization’s 2021 guidance on AI ethics in health.
Sources
- De Fauw, J., et al. (2018). Clinically applicable deep learning for diagnosis and referral in retinal disease. Nature Medicine. https://www.nature.com/articles/s41591-018-0107-6
- McKinney, S. M., et al. (2020). International evaluation of an AI system for breast cancer screening. Nature. https://www.nature.com/articles/s41586-019-1799-6
- Aidoc (2023). Case Studies and Clinical Impact. https://www.aidoc.com/resources/
- Tschandl, P., et al. (2020). Human–computer collaboration for skin cancer recognition. The Lancet Digital Health. https://www.thelancet.com/journals/landig/article/PIIS2589-7500(19)30200-8/fulltext
- Zhou, Y., et al. (2021). AI in drug discovery: Insights and challenges. Drug Discovery Today. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8056493/
- Senior, A. W., et al. (2020). AlphaFold: Protein structure prediction. Nature. https://www.nature.com/articles/s41586-020-2649-2
- Fauver, J. R., et al. (2021). Neuroadaptive therapy platforms in mental health. PubMed. https://pubmed.ncbi.nlm.nih.gov/34545342/
- Obermeyer, Z., et al. (2019). Dissecting racial bias in an algorithm used to manage population health. Science. https://www.science.org/doi/10.1126/science.aax2342
- Doshi-Velez, F., & Kim, B. (2017). Towards a rigorous science of interpretable machine learning. https://arxiv.org/abs/1702.08608
- FDA (2020). Software as a Medical Device (SaMD). https://www.fda.gov/medical-devices/digital-health-center-excellence/software-medical-device-samd
- Stanford Medicine (2023). Health Trends Report. https://med.stanford.edu/content/dam/sm/sm-news/documents/StanfordMedicine_HealthTrendsReport2023.pdf
- Singhal, K., et al. (2022). Med-PaLM: Large Language Models in Medicine. https://arxiv.org/abs/2302.07081
- Guntuku, S. C., et al. (2017). Detecting mental health from social media. Journal of Medical Internet Research. https://www.jmir.org/2017/5/e75/
The article does not in any way constitute as medical advice. Please seek consultation with a licensed medical professional before starting any treatment. This website may receive commissions from the links or products mentioned in this article.
Subscribe for Free for more insightful health articles tailored to your needs.