
By Samantha Grant, Cognitive Hypnotherapist, Anxiety & Stress Specialist|Published on August 26, 2025

You’re exhausted all day — but the moment you try to sleep, your mind switches on.
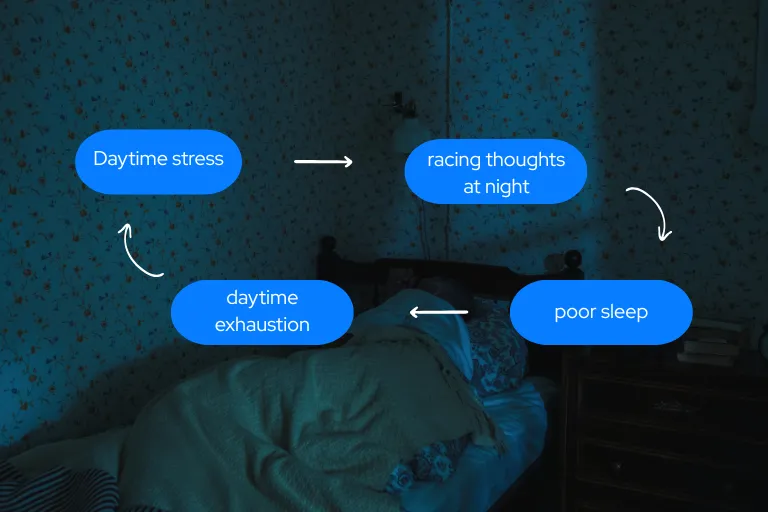
It’s a cycle millions know too well.
By mid-morning, you’re yawning over coffee. By late afternoon, you’re counting the hours until bed. But when you finally lie down, your body feels tense, your mind races, and you’re wide awake for hours.
This frustrating state — tired but wired — is more than a quirk of personality or bad sleep habits. It’s often a sign your body’s stress-response system is stuck in high gear… even when you’re trying to rest.
When You’re Doing Everything Right — But Still Can’t Sleep

In my work as a Cognitive Hypnotherapist, I help people resolve anxiety, stress, insomnia, and low mood using a combination of:
- Hypnotherapy
- Psych-K
- NLP
These methods help reprogramme subconscious patterns — shifting how people feel, think, and behave — so they can move naturally from tension into calm.
Most of my clients see their sleep improve significantly after therapy alone. But every so often, I meet someone who still struggles to switch off, even when their conscious mind is ready.
What I’ve Noticed in Over a Decade of Helping People Sleep
Across hundreds of clients, there’s a small group who:
- Manage their stress well during the day
- Practice good “sleep hygiene”
- Have tried everything from herbal teas to meditation apps
…and yet, when night comes, their body feels wired — as if it hasn’t received the “time to rest” signal.
These are the clients who often benefit from extra support between sessions — something to help their body’s recovery systems work with the mind, not against it.
The Science Behind ‘Tired But Wired’
The human nervous system has two main modes:
- Sympathetic (“fight or flight”) — alert, energised, ready for action
- Parasympathetic (“rest, digest, repair”) — calm, restorative, deep sleep
Ideally, we move between them with ease. But prolonged stress — even subtle, background stress — can trap the body in a state of sympathetic dominance.
The result?
- Racing thoughts at bedtime
- Frequent night-time awakenings
- Morning grogginess, even after 8 hours in bed
- A sense of being “on alert” all the time
This is not laziness or poor discipline. It’s a biological state — and one particular nerve plays a crucial role in shifting it.
The Vagus Nerve — Your Body’s Calm Switch
The vagus nerve is the main pathway of the parasympathetic nervous system, running from your brainstem to your heart, lungs, and digestive organs.
When the vagal tone is strong, your body can switch easily into a restorative state. When it’s weak, the “off switch” for stress is harder to find — even if you feel exhausted.

Low vagal tone has been linked in research to:
- Fragmented sleep
- Increased inflammation
- Higher anxiety
- Reduced stress resilience
Why This Matters for Sleep
Your body doesn’t sleep just because you close your eyes. It sleeps when it feels safe enough to let go.
If your nervous system is on high alert, your heart rate may stay slightly elevated, your muscles slightly tensed, and your brain on standby for potential threats — all of which disrupt the deep stages of sleep.
This is why some people wake feeling like they’ve barely slept, even if their tracker shows 7–8 hours in bed.
Supporting the Nervous System — Beyond Sleep Hygiene
Many people try breathwork, meditation, or gentle stretching before bed.
These can help — but they rely on daily consistency and may take weeks before the body adapts.
In recent years, I’ve taken interest in a more direct approach:
Transcutaneous Auricular Vagus Nerve Stimulation (taVNS) — a gentle, non-invasive method of stimulating the vagus nerve via the skin of the ear.
Where Nurosym Fits (At-Home Support)

I first tried Nurosym myself for menopausal sleep disruptions, digestive discomfort, and frequent night-time waking.
While my symptoms varied for other reasons too, I found the sessions deeply relaxing — enough that I began suggesting it to select clients.
My main work focuses on resolving the root causes through therapy. But for clients who need extra nervous system support between sessions — especially during stressful life events — Nurosym can be a useful complement.
What the Research Says
Nurosym is a CE-marked taVNS medical device used in more than 50 clinical studies, including collaborations with Harvard, Yale, and Imperial College London.
Published studies have found that taVNS can:
- Improve heart rate variability (HRV) — a measure of nervous system balance
- Reduce inflammatory markers like IL-6 and TNF-alpha
- Improve subjective sleep quality in people with disrupted sleep patterns
- Lower stress reactivity and promote relaxation
In my practice, clients have described benefits such as:
“I fall asleep faster, even on stressful days.”
“I wake up less during the night and feel calmer in the morning.”
Who Might Benefit
- People who feel tired but wired most nights
- Those whose insomnia worsens during stressful periods
- Clients in therapy who want extra between-session support for relaxation
- People waking frequently despite good sleep hygiene
Who Shouldn’t Use It
Nurosym (and taVNS generally) should be avoided if you:
- Have a pacemaker or implantable cardiac device
- Are pregnant
- Have had a recent serious cardiac event
- Are under 18
Always check with a qualified health professional before starting.
A Safe Way to Try It
- 30-Day Money-Back Guarantee — Start your 30-day home trial today — with a money-back guarantee if you don’t notice deeper, calmer sleep.
- Limited Study Slots — at times, participants may receive a ~€70 subsidy for sharing their experience
I guide clients on whether it’s suitable, how to use it correctly, and how to combine it with therapy for the best results.

Final Thoughts — Rest Isn’t Always Recovery
If you’ve tried every sleep tip but still feel wired at night, it’s not about willpower — it’s about helping your nervous system feel safe enough to rest.
Through targeted therapy, it’s possible to retrain your body’s stress-response patterns. And for some, tools like Nurosym can provide that extra nudge toward deep, restorative sleep.
If you’ve tried everything else and still feel wired at night, see how Nurosym can help you finally feel safe enough to rest.
References:
- Chalmers, J. A., Quintana, D. S., Abbott, M. J.-A., & Kemp, A. H. (2014). Anxiety disorders are associated with reduced heart rate variability: A meta-analysis. Frontiers in Psychiatry, 5, 80. https://doi.org/10.3389/fpsyt.2014.00080
- Chouchou, F., & Desseilles, M. (2014). Heart rate variability: A tool to explore the sleeping brain? Frontiers in Neuroscience, 8, 402. https://doi.org/10.3389/fnins.2014.00402
- Cooper, T. M., McKinley, P. S., Seeman, T. E., Choo, T.-H., Lee, S., & Sloan, R. P. (2015). Heart rate variability predicts levels of inflammatory markers: Evidence for the vagal anti-inflammatory pathway. Brain, Behavior, and Immunity, 49, 94–100. https://doi.org/10.1016/j.bbi.2014.12.017
- Kim, A. Y., Marduy, A., de Melo, P. S., Gianlorenco, A. C., Kim, C. K., Choi, H., Song, J. J., & Fregni, F. (2022). Safety of transcutaneous auricular vagus nerve stimulation (taVNS): A systematic review and meta-analysis. Scientific Reports, 12, 22055. https://doi.org/10.1038/s41598-022-25864-1
- Palesh, O., Zeitzer, J. M., Conrad, A., Giese-Davis, J., Mustian, K. M., Popek, V., Nga, K., & Spiegel, D. (2008). Vagal regulation, cortisol, and sleep disruption in women with metastatic breast cancer. Journal of Clinical Sleep Medicine, 4(5), 441–449. https://doi.org/10.5664/jcsm.27280
- Ylikoski, J., et al. (2020). Stress and tinnitus: Auricular vagus nerve stimulation attenuates tinnitus-triggered stress reaction. Frontiers in Psychology, 11, 570196. https://doi.org/10.3389/fpsyg.2020.570196
- Zhang, S., et al. (2024). Transcutaneous auricular vagus nerve stimulation for chronic insomnia disorder: A randomized clinical trial. JAMA Network Open, 7(12), e2451217. https://doi.org/10.1001/jamanetworkopen.2024.51217
- Bremner, J. D., et al. (2020). Transcutaneous vagal nerve stimulation blocks stress-induced IL-6 and IFN-γ in posttraumatic stress disorder: A double-blind, randomized, sham-controlled trial. Brain, Behavior, & Immunity – Health, 9, 100138. https://doi.org/10.1016/j.bbih.2020.100138
The article does not in any way constitute as medical advice. Please seek consultation with a licensed medical professional before starting any treatment. This website may receive commissions from the links or products mentioned in this article.
Share via:


