A comprehensive review of how VNS devices address post-viral autonomic dysfunction—with expert rankings of the top 4 certified options.

Long COVID, formally termed Post-Acute Sequelae of SARS-CoV-2 Infection (PASC), affects an estimated 7.5% of US adults who contracted COVID-19—representing tens of millions globally. Unlike acute COVID-19, PASC manifests as persistent, often debilitating symptoms extending months or years beyond initial infection, despite viral clearance.
Emerging research suggests that autonomic nervous system dysfunction, including impaired vagal activity, may contribute to symptom persistence in a subset of individuals with Long COVID, alongside other mechanisms such as immune dysregulation, endothelial dysfunction, viral persistence, and metabolic impairment. When SARS-CoV-2 infection damages this cranial nerve—either through direct viral neurotropism, inflammatory injury, or autoimmune activation—individuals experience dysregulation across multiple organ systems regulated by vagal pathways.
This guide examines the mechanistic relationship between vagus nerve dysfunction and Long COVID symptomatology, and evaluates the leading vagus nerve stimulation (VNS) devices that may facilitate autonomic recovery and symptom resolution.
Symptoms of Long COVID
Post-Acute Sequelae of SARS-CoV-2 Infection encompasses a heterogeneous constellation of symptoms persisting beyond 12 weeks from initial infection. Research identifies over 200 documented symptoms across multiple organ systems:
Cardiopulmonary manifestations:
- Dyspnea (shortness of breath) disproportionate to exertion level
- Chest tightness, pressure, or pain
- Rapid heartbeat or palpitations at rest or with minimal activity
- Exercise intolerance with oxygen desaturation
- Persistent cough without pulmonary pathology on imaging
- Orthostatic intolerance (symptoms worsening when upright)
Neurological manifestations:
- Cognitive dysfunction ("brain fog"): impaired executive function, processing speed, working memory
- Post-exertional cognitive impairment lasting 24-72 hours
- Headaches (often tension-type or migraine variants)
- Peripheral neuropathy (paresthesias, dysesthesias)
- Dysautonomia (temperature dysregulation, inappropriate sweating)
- Sleep architecture disruption (non-restorative sleep, sleep problems)
Systemic inflammatory symptoms:
- Profound fatigue unrelieved by rest
- Post-exertional malaise (symptom exacerbation following physical or cognitive activity)
- Myalgias (muscle pain) and arthralgias (joint pain)
- Persistent low-grade fever or temperature instability
- Lymphadenopathy without active infection
Gastrointestinal manifestations:
- Nausea or reduced appetite
- Gastrointestinal dysmotility (gastroparesis symptoms, constipation, diarrhoea)
- Abdominal discomfort or pain
- Dysgeusia (altered taste) or dysosmia (altered smell)
Additional manifestations:
- Anxious thoughts or mood disturbances (often secondary to chronic symptoms)
- Menstrual cycle irregularities
- Tinnitus (ringing in the ears)
- Visual disturbances
- New-onset allergic responses or mast cell activation symptoms
The functional consequences extend beyond symptomatology: studies show 22-27% of Long COVID individuals report significant work impairment, with many unable to return to pre-infection employment levels, experiencing educational disruption, financial strain from health expenses, and marked deterioration in quality of life indices.

Long COVID Self-Assessment
Evaluate symptoms you have experienced persistently for ≥12 weeks following confirmed or suspected SARS-CoV-2 infection:
Cardiopulmonary Function
- Shortness of breath during routine activities, previously well-tolerated
- Chest pain, tightness, or pressure
- Heart palpitations or awareness of a rapid heartbeat
- Difficulty taking deep breaths
- Symptoms worsen with physical exertion
Cognitive Function
- Difficulty concentrating or "brain fog"
- Memory problems (short-term recall, word-finding difficulty)
- Mental tasks require substantially more effort than pre-infection
- Cognitive symptoms worsen after mental exertion
- Reduced processing speed or "thinking through fog"
Energy & Post-Exertional Response
- Profound fatigue not improved with rest
- "Crashes" or severe symptom worsening 12-48 hours after activity
- The energy envelope is severely restricted compared to pre-infection
- Must carefully ration physical and cognitive activities
- Recovery from exertion takes days, not hours
Autonomic Symptoms
- Temperature regulation problems (feeling too hot or cold inappropriately)
- Excessive sweating or inability to sweat normally
- Dizziness or lightheadedness, especially when standing
- Gastrointestinal disturbances (nausea, appetite changes, altered motility)
- Sleep disruption despite exhaustion
Sensory & Neurological
- Headaches (new onset or changed pattern)
- Tingling, numbness, or burning sensations
- Tinnitus or ear pressure
- Altered taste or smell (beyond initial infection period)
- Hypersensitivity to sensory stimuli
Functional Impact
- Unable to work at pre-infection capacity
- Social activities severely limited
- Household tasks require rest periods
- Symptoms fluctuate unpredictably
- Multiple health professional consultations without a definitive diagnosis
Medical History
- Symptoms began during or shortly after the COVID-19 infection
- Standard scientific testing (labs, imaging) is largely unremarkable
- Symptoms persist despite "full recovery" from acute infection
- Vaccination status does not correlate with symptom resolution
- Multiple specialists consulted without a comprehensive explanation
If you identify with 12+ items, particularly across Cardiopulmonary, Cognitive, and Post-Exertional categories, you may be experiencing Long COVID with features suggestive of autonomic involvement, which warrants evaluation by a clinician familiar with post-viral syndromes.
Vagus nerve stimulation warrants consideration as an adjunctive intervention in consultation with your healthcare provider.
The Vagus Nerve Connection: Why This Nerve Controls Your Recovery
What Is the Vagus Nerve?
The vagus nerve is the longest nerve in your body—a biological superhighway connecting your brain to virtually every major organ. It runs from your brainstem down through your neck and chest into your abdomen.
Think of it as your body’s master control cable. It continuously sends signals between your brain and organs. Here’s what makes it remarkable: 80% of these signals travel FROM your organs TO your brain—meaning the vagus nerve is your body’s primary system for monitoring your internal state.
This nerve controls the organ systems that directly relate to Long COVID symptoms:
- Cardiovascular system — controls heart rate and blood flow → explains heart palpitations, chest tightness, exercise intolerance.
- Pulmonary system — regulates breathing rhythm → explains shortness of breath and air hunger despite normal oxygen levels.
- Gastrointestinal tract — manages digestion and gut movement → explains nausea, stomach problems, and altered bowel habits.
- Immune system — controls inflammation response → explains persistent inflammation driving fatigue, pain, and widespread symptoms.
- Energy metabolism — regulates glucose and energy production → explains energy crashes and metabolic dysfunction.
- Brain function — connects to thinking and memory centres → explains brain fog, cognitive impairment, difficulty concentrating.
When SARS-CoV-2 infection is associated with impaired vagal signalling, whether through inflammatory, immune-mediated, or neurovascular mechanisms, individuals may experience multi-system autonomic dysregulation.
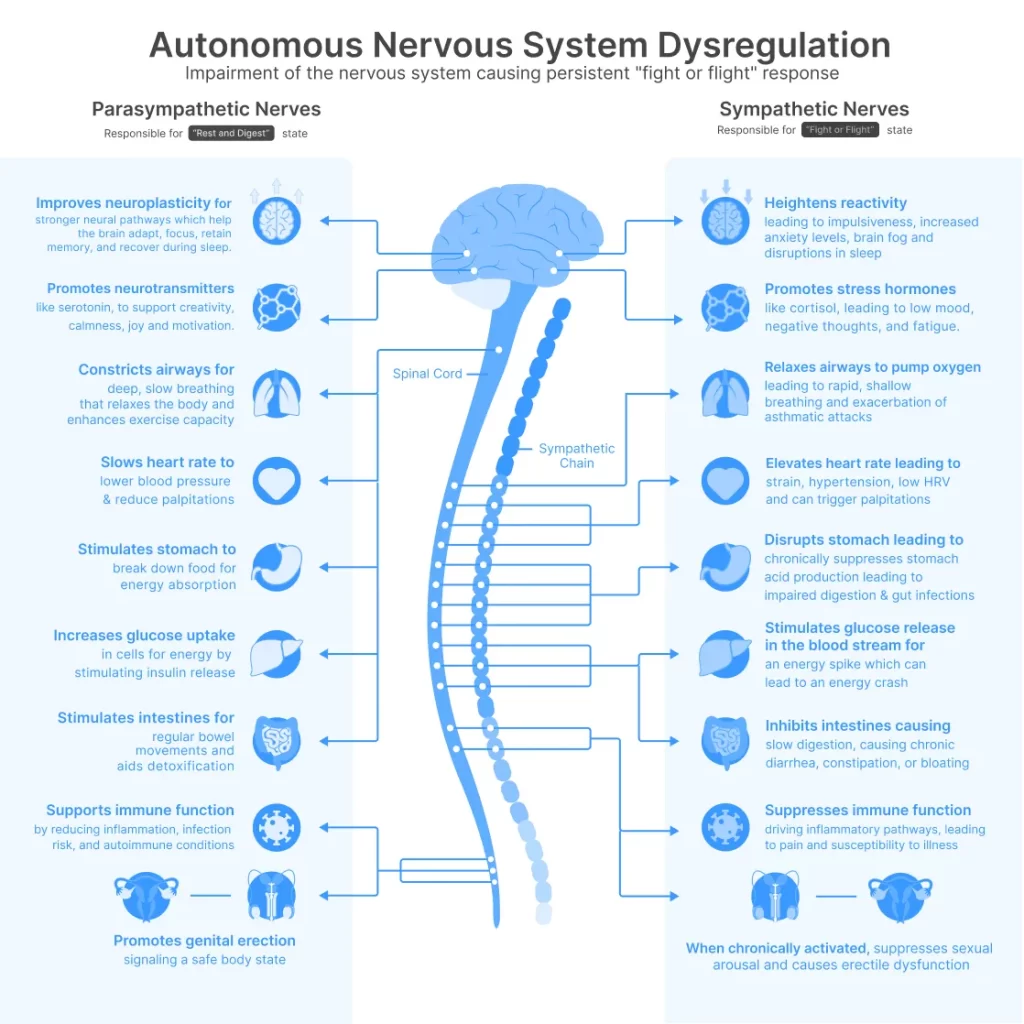
The Two-Mode System: Stuck in Emergency Mode
Your nervous system has two modes that should work together, switching based on what your body needs:
- Sympathetic — "Fight or Flight": Increases heart rate and blood pressure, redirects energy to muscles, heightens alertness, releases stress hormones. This mode helps you handle emergencies—sprint from danger or meet a deadline. It's designed for brief threats, not constant use. When it stays active too long, it becomes physically damaging.
- Parasympathetic — "Rest and Digest": Controlled by the vagus nerve, this mode slows heart rate, supports digestion, promotes tissue repair, enables restorative sleep, and activates anti-inflammatory pathways. This is your healing mode—essential for recovery and long-term health.
The Long COVID Trap
In a healthy person, your nervous system switches between these modes as needed.
Threat appears? Sympathetic mode activates.
Threat passes? Parasympathetic mode restores you.
In some individuals, COVID-19 may impair vagal signalling, disrupting the body’s ability to shift back into parasympathetic (“healing”) mode. You become trapped in sympathetic dominance—stuck in emergency status even while lying in bed trying to rest.
This explains the Long COVID paradox: profound exhaustion yet racing heart rate, desperate need for sleep yet non-restorative rest, hunger for recovery yet a body stuck in stress response. Your vagus nerve—the switch that should activate healing—is damaged and can’t do its job.
Without adequate vagal activity, you experience:
- Cardiovascular symptoms: Racing heart, palpitations, unstable blood pressure—your heart lacks its parasympathetic brake.
- Respiratory dysfunction: Air hunger despite normal oxygen—vagal breathing regulation is impaired.
- Cognitive impairment: Brain fog and memory problems—vagal connections to thinking centres are compromised.
- Chronic tiredness: Exhaustion that rest doesn't fix—you literally cannot shift into restorative mode.
- Post-exertional malaise: Days-long crashes after minimal activity—your recovery system doesn't work.
- Persistent inflammation: Ongoing symptoms despite viral clearance—the vagal anti-inflammatory pathway stays suppressed.
- Sleep dysfunction: Non-restorative sleep despite hours in bed—vagal tone doesn't increase during sleep as like it should.
The Real Problem
This isn’t about needing to “push through” or “manage stress better.” The problem is neurological: your vagus nerve is damaged, and your nervous system can’t switch into healing mode.
This is why conventional therapies that address individual symptoms separately—anxious thoughts medication here, pain relief there, fatigue management somewhere else—provide minimal relief. They treat downstream effects while the upstream control system remains broken.
Supporting vagal function may be an important component of recovery for some individuals with Long COVID. When vagal activity is restored, your nervous system regains the ability to shift out of sympathetic overdrive and into the parasympathetic healing state, where actual recovery becomes possible.
It is important to emphasise that Long COVID is a heterogeneous state. Not all individuals exhibit measurable autonomic dysfunction, and vagal impairment does not explain every symptom. Multidisciplinary care addressing cardiovascular, pulmonary, neurological, metabolic, and psychological dimensions remains essential. Neuromodulation approaches should be considered adjunctive, not replacement, therapies.

How SARS-CoV-2 Damages the Vagus Nerve
Emerging research identifies several pathways through which COVID-19 impairs vagal function:
- Direct viral neurotropism: SARS-CoV-2 exhibits affinity for ACE2 receptors expressed on neurons and glial cells. The virus can access the central nervous system via olfactory, trigeminal, and vagal routes. Viral particles have been detected in the vagus nerve and brainstem nuclei in autopsy studies, suggesting direct neural invasion.
- Inflammatory-mediated injury: Acute COVID-19 triggers cytokine storm with elevated IL-6, IL-1β, and TNF-α. These pro-inflammatory mediators can damage neural tissue, including vagal fibres. Persistent low-grade inflammation in Long COVID continues this injury process.
- Autoimmune activation: Post-infection, some individuals develop autoantibodies targeting autonomic receptors (α/β-adrenergic, muscarinic cholinergic). These autoantibodies can disrupt normal vagal signalling and perpetuate autonomic dysfunction.
- Microvascular damage: COVID-19 causes endothelial dysfunction and microclots, potentially disrupting blood supply to the vagus nerve (vasa nervorum), leading to ischemic injury.
- Viral reservoir hypothesis: Emerging research suggests SARS-CoV-2 may persist in anatomical reservoirs (including the gut, where vagal innervation is extensive), maintaining chronic immune activation and ongoing vagal dysfunction.
How Vagus Nerve Dysfunction Causes Long COVID Symptoms
When vagal tone is compromised following SARS-CoV-2 infection:
- Cardiovascular dysregulation: Loss of parasympathetic counterbalance causes a resting rapid heartbeat, orthostatic intolerance, and exercise intolerance. Individuals experience inappropriate heart rate elevation with minimal exertion because vagal "braking" mechanisms are impaired. Heart rate variability—a validated biomarker of vagal activity—is markedly reduced in Long COVID individuals.
- Respiratory dysfunction: The vagus nerve regulates respiratory rhythm and bronchial tone. Dysfunction contributes to dyspnea (air hunger sensation) even with normal oxygen saturation and clear chest imaging. Individuals describe feeling unable to take satisfying deep breaths—a phenomenon linked to vagal afferent signalling disruption.
- Cognitive impairment: Ascending vagal projections to brainstem nuclei (nucleus tractus solitarius, locus coeruleus) influence arousal, attention, and memory consolidation. Reduced vagal activity correlates with cognitive dysfunction. Additionally, impaired cerebral blood flow autoregulation—partly vagally mediated—may contribute to brain fog.
- Post-exertional malaise: This cardinal Long COVID feature reflects autonomic failure to shift appropriately between energy expenditure and recovery states. Without adequate vagal activation, the parasympathetic "rest and digest" mode doesn't engage properly after exertion, preventing metabolic recovery and perpetuating sympathetic overdrive.
- Gastrointestinal symptoms: The vagus nerve provides parasympathetic innervation to a big portion of the GI tract, regulating motility, secretion, and gut-brain communication. Vagal dysfunction causes gastroparesis-like symptoms, nausea, altered bowel habits, and contributes to dysbiosis (microbiome alterations documented in Long COVID).
- Immune dysregulation: The cholinergic anti-inflammatory pathway represents a critical vagal function. Through splenic nerve signalling, vagal activation suppresses pro-inflammatory cytokine production. When this pathway is impaired, chronic low-grade inflammation persists—documented in Long COVID individuals with elevated CRP, IL-6, and other markers. This inflammation drives fatigue, pain, and multi-system symptoms
- Sleep disruption: Vagal tone normally increases during sleep, facilitating restoration. In Long COVID, individuals show reduced overnight vagal activity, preventing restorative sleep architecture. Despite spending 8-10 hours in bed, they wake exhausted because true physiological recovery doesn't occur.

The Scientific Evidence
The Scientific Evidence: Emerging Data on Vagal Dysfunction and Neuromodulation
Published research increasingly suggests that vagal dysfunction may contribute to Long COVID symptomatology and that targeted neuromodulation may help modulate related physiological processes.
The Problem Documented:
- Long COVID individuals show significantly reduced heart rate variability compared to recovered individuals—indicating vagal impairment that correlates with symptom severity.
- Autonomic dysfunction explains the cardiovascular instability, exercise intolerance, and post-exertional crashes that devastate daily function.
- Elevated inflammatory markers drive the persistent fatigue and brain fog—resulting from impaired vagal regulation of the immune response.
- Research shows COVID-19 impairs vagus nerve function, leading to dysautonomia (autonomic nervous system imbalance).
Scientific Studies Prove VNS Works:
- Preliminary scientific studies and pilot studies suggest that transcutaneous vagus nerve stimulation may improve selected symptoms in some individuals with Long COVID, particularly fatigue, autonomic instability, and inflammatory markers.
- These studies are generally small, short-term, and heterogeneous in design.
- Reported outcomes include reductions in fatigue scores, improvements in autonomic measures such as heart rate variability, and modulation of inflammatory biomarkers.
- However, these findings require confirmation in larger, randomised, controlled studies before definitive conclusions can be drawn.
- Current evidence supports VNS as a potential adjunctive neuromodulatory approach, not a standalone or curative solution for Long COVID.
Top 4 VNS Devices for Long COVID
#1: Nurosym
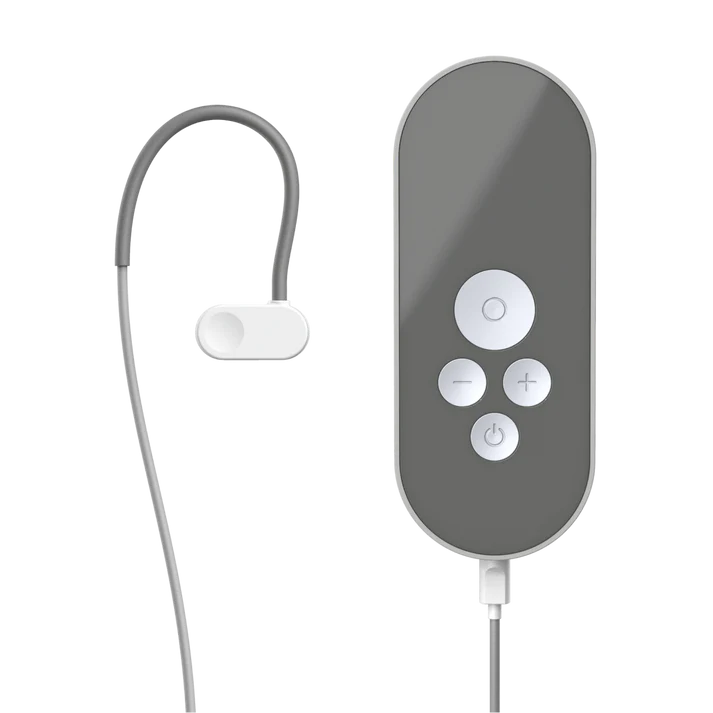
Price: 700 EUR (€70 research subsidy available for Long COVID individuals)
Type: Auricular (ear-worn)
Technology: AVNT™ by Parasym
Why #1:
- Most extensively validated: Supported by 50+ peer-reviewed publications from University College London, UCLA, and the University of Chicago and leading research institutions worldwide.
- Proven efficacy for Long COVID: Scientific studies document 61% overall symptom improvement, 48% fatigue reduction, 78% reduction in inflammatory markers, 40% improvement in post-COVID Postural Heart Rate Abnormalities symptoms—directly targeting the autonomic dysfunction and neuroinflammation driving persistent post-viral illness.
- Independent certification: CE-marked wearable device meeting rigorous safety and performance standards—third-party verified.
- Scientific adoption: Used by 1,000+ healthcare professionals treating post-viral syndromes; integrated into Long COVID rehabilitation protocols; 4,000,000+ stimulation sessions completed.
- Evidence-based parameters: Stimulation protocols derived from peer-reviewed fatigue research, not proprietary guesswork.
- Comprehensive support: 30-day money-back guarantee, scientific guidance resources, responsive technical support, and ongoing research participation opportunities.
Best for: Long COVID individuals seeking the most scientifically validated device with published scientific studies demonstrating efficacy for post-viral autonomic dysfunction, fatigue, brain fog, and inflammatory symptoms.
#2: Truvaga Plus

Price: $544+ (device $499 + spray $45/year + potential subscription) Type: Cervical (neck handheld)
Technical note: Shares core technology with gammaCore, an FDA-cleared device for migraine/cluster headache (not Long COVID). Rapid parasympathetic effects. Straightforward protocol.
Considerations: Ongoing costs for conductive spray plus potential app subscription—verify pricing before purchase. Common adverse effects include muscle spasms, facial droop, lip pull, and headache. Not suitable for users with cardiac state, pacemakers, or recent heart issues—relevant for Long COVID individuals with cardiovascular complications. Mobile app connectivity problems reported.
Best for: Those preferring cervical stimulation with FDA-cleared technology lineage (for migraine, not Long COVID) who can tolerate potential facial muscle spasm adverse effects.
#3: Pulsetto

Price: $350-$371 (device $269 + gel $81-$102/year) Type: Cervical (hands-free collar)
Advantages: Hands-free wearable design. HSA/FSA eligible. 2-year warranty coverage.
Critical Limitations: No peer-reviewed scientific studies demonstrating efficacy for Long COVID or post-viral syndromes—only company press releases and retail testimonials. Frequent fit problems create inadequate nerve contact, especially with smaller necks. Users consistently report minimal to no improvement in Long COVID symptoms compared to research-validated devices.
Not recommended for Long COVID: The $200-350 price difference seems attractive until you calculate the real cost: months of continued post-viral disability while using an unproven device. After already losing months or years to Long COVID, can you afford to gamble more time on a device without scientific evidence? Lower-cost devices may be appealing; however, the absence of peer-reviewed scientific evidence for post-viral syndromes limits confidence in their effectiveness. Individuals prioritising evidence-based approaches may prefer devices with published scientific data.
#4: Sensate

Price: $299-$349 Type: Chest-worn vibrotactile device (not true VNS)
Advantages: Comfortable pebble design worn on the chest. Simple app interface with soundscapes. Lower price point. Can be used while performing other activities with the neck strap.
Critical distinction: Sensate does not directly stimulate the vagus nerve through electrical impulses like other devices in this comparison. Instead, it uses infrasonic vibrations and bone conduction placed on the chest—an indirect approach targeting general stress reduction rather than specific vagal nerve activation. While bone conduction at the ear has some research supporting vagal stimulation, Sensate’s chest placement lacks scientific substantiation for direct vagus nerve engagement. The mechanism is fundamentally different: actual VNS devices (like Nurosym, Truvaga, or Pulsetto) deliver calibrated electrical signals directly to accessible vagus nerve branches; Sensate delivers vibrations to your sternum, with indirect downstream physiological effects that are not yet well-characterised in the post-viral state.
For Long COVID individuals: This matters significantly. Long COVID requires restoration of measurable autonomic function—reduced inflammation, normalised immune response, improved energy metabolism, enhanced cognitive function. General relaxation devices may help with stress management, but do not address the underlying vagal dysfunction, neuroinflammation, and immune dysregulation driving Long COVID symptoms. No scientific studies demonstrate Sensate’s efficacy for Long COVID or post-viral syndromes—only company-funded studies showing general stress reduction in healthy volunteers.
Best for: Those seeking a general relaxation and stress management tool rather than targeted vagus nerve stimulation for post-viral recovery. Not recommended for individuals prioritising evidence-based Long COVID therapy.
*€70 research subsidy available for qualifying participants contributing to ongoing scientific research protocols
**All devices require careful attention to manufacturer protocols; individual responses vary based on underlying pathophysiology and adherence
Nurosym provides the most comprehensive scientific validation, documented efficacy for autonomic dysfunction, including Long COVID presentations, independent regulatory certification through a rigorous CE-marking process, and optimal integration of research foundation with practical accessibility for individuals prioritising evidence-based interventions.
Take Action
In some individuals, Long COVID associated with autonomic dysfunction may be partially modifiable through targeted neuromodulation and supportive interventions. Your autonomic nervous system retains capacity for recovery through targeted neuromodulation and neuroplastic adaptation.
With validation from 60+ peer-reviewed studies, independent CE-marking certification, and 4,000,000+ documented stimulation sessions, Nurosym offers scientifically grounded potential for autonomic recovery and restoration of functional capacity.
30-day evaluation period. Validated by 60+ scientific studies.
This information is provided for educational purposes regarding autonomic dysfunction in post-viral syndromes. VNS devices are not intended to diagnose, treat, cure, or prevent any disease. Long COVID individuals should work with qualified healthcare providers to develop comprehensive, individualised management strategies. Consultation with your physician is essential before initiating any new intervention, particularly for complex post-viral presentations.
Disclaimer: This blog post aims to be informational and should not replace professional health advice. Always consult with a health professional for personalised advice.
Sources
- Khan MWZ, Ahmad M, Qudrat S, Afridi F, Khan NA, Afridi Z, et al. Vagal nerve stimulation for the management of long COVID symptoms. Infectious Medicine [Internet]. 2024 Nov 8;100149. Available from: https://www.sciencedirect.com/science/article/pii/S2772431X24000637
- Basharat S, Mahood Q. Vagus Nerve Stimulation for the Treatment of Post–COVID-19 Condition. Canadian Journal of Health Technologies. 2022 Sep 20;2(9).
- Zheng ZS, Simonian N, Wang J, Rosario ER. Transcutaneous vagus nerve stimulation improves Long COVID symptoms in a female cohort: a pilot study. Frontiers in Neurology. 2024 May 2;15.
- Gierthmuehlen M, Gierthmuehlen PC. COVIVA: Effect of transcutaneous auricular vagal nerve stimulation on fatigue-syndrome in patients with Long Covid – A placebo-controlled pilot study protocol. PLoS ONE. 2025 May 9;20(5):e0315606–6.
- Pfoser-Poschacher V, Keilani M, Steiner M, Schmeckenbecher J, Zwick RH, Crevenna R. Feasibility and acceptance of transdermal auricular vagus nerve stimulation using a TENS device in females suffering from long COVID fatigue. Wiener klinische Wochenschrift. 2025 Feb 19;137(19-20):635–41.
- Lladós G, Massanella M, Coll-Fernández R, Rodríguez R, Hernández E, Lucente G, et al. Vagus Nerve Dysfunction in the Post-COVID-19 Condition: a pilot cross sectional study. Clinical Microbiology and Infection [Internet]. 2023 Nov 19 [cited 2023 Nov 25]; Available from: https://www.sciencedirect.com/science/article/pii/S1198743X23005657
Share via:


