A higher HRV means better stress resilience, deeper sleep, and faster recovery. Here’s what actually works, and what the science says.

Why Your HRV Matters More Than You Think
If you’re tracking your heart rate variability, you already know something important: your body is trying to tell you something.
Maybe your HRV has been trending downward for weeks. Or perhaps you noticed it drops after stressful days, poor sleep, or intense workouts. You’re not imagining it, these patterns are real signals from your nervous system.
Heart rate variability measures the tiny changes in time between your heartbeats. When that variability is high, it means your body can adapt. It can shift from “go mode” to “rest mode” smoothly. It recovers faster and it handles stress better.
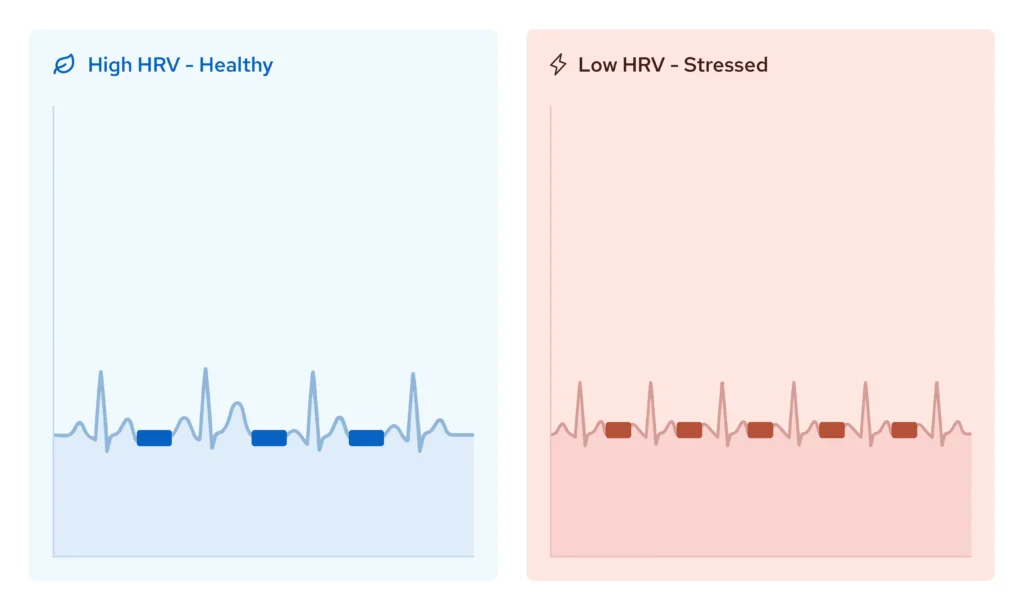
When HRV is low? Your nervous system is stuck. You feel it as exhaustion that sleep doesn’t fix. Anxious thoughts that won’t quiet. Recovery that takes days instead of hours.
The good news: HRV isn’t fixed. It responds to how you support your nervous system. And unlike most health metrics, you can measure changes in real time, right there on your wrist.
This guide explains what actually improves HRV, according to science. Not wellness trends. Not guesswork. Just the interventions that have been studied, measured, and proven to work.
What HRV Actually Measures (And Why It Matters)
Heart rate variability isn’t about your heart rate: it’s about the space between beats.
Your nervous system has two main modes:
- Sympathetic ("fight-or-flight"): Active, alert, stress-responsive
- Parasympathetic ("rest-and-digest"): Calm, recovery, restoration
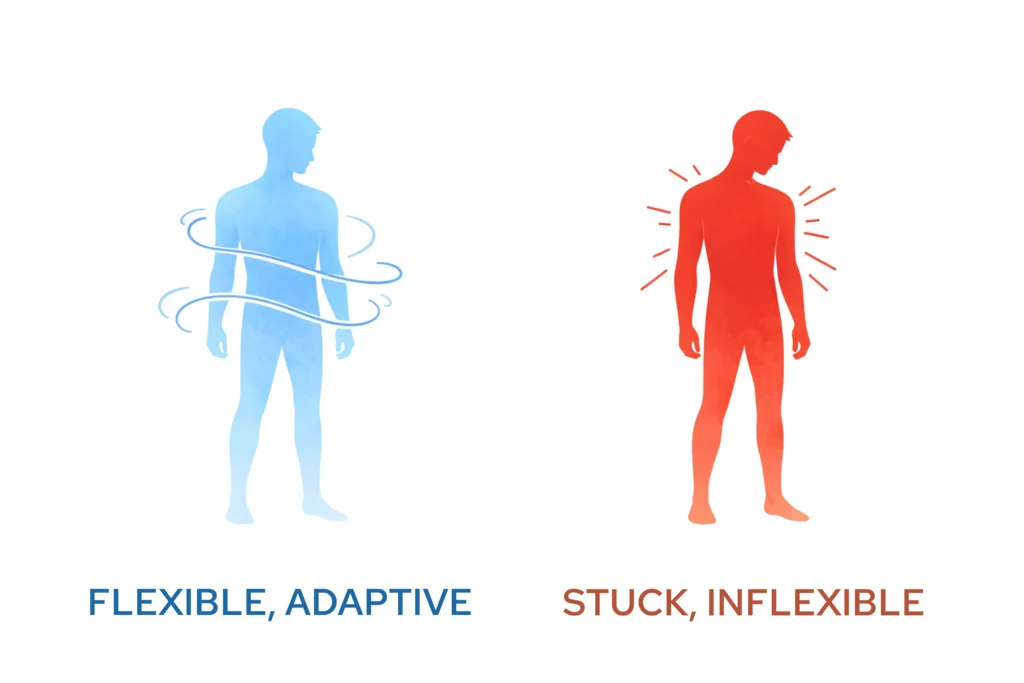
A healthy nervous system switches between these modes smoothly. When you need to focus or respond to stress, your sympathetic system activates. When the moment passes, your parasympathetic system takes over to rest and recover.
HRV measures how well this system is working.
High HRV means your nervous system is flexible.
→ The space between heartbeats varies more because your body is adapting moment to moment. This is a sign of resilience.
Low HRV means your nervous system is rigid.
→ The space between beats becomes more uniform, often because you’re stuck in sympathetic overdrive. This shows up as poor recovery, persistent fatigue, or difficulty managing stress.
Your autonomic nervous system controls functions you don’t consciously think about: breathing, heart rate, digestion, energy levels, mood regulation. When it’s dysregulated, everything feels harder.
That’s why HRV matters: it’s a window into whether your nervous system is functioning well, or struggling.
The Root Cause: A Dysregulated Nervous System
Most advice about improving HRV focuses on lifestyle: sleep better, stress less, exercise moderately. These things help, but they don’t address why your nervous system became dysregulated in the first place.
Modern life keeps most people in chronic sympathetic activation.
- Work stress.
- Screen time.
- Poor sleep.
- Constant stimulation.
Your body stays in “fight-or-flight” mode, rarely dropping into true rest.
Over time, this becomes the baseline. Your parasympathetic system (the brake pedal that should activate recovery) stops engaging properly.
The result? Low HRV. And all the symptoms that come with it:
- Waking up tired despite sleeping 7-8 hours
- Difficulty calming down after stress
- Feeling "wired but tired"
- Slow recovery after exercise
- Brain fog or reduced focus
- Anxious thoughts or mood swings
Here’s what most people don’t know:
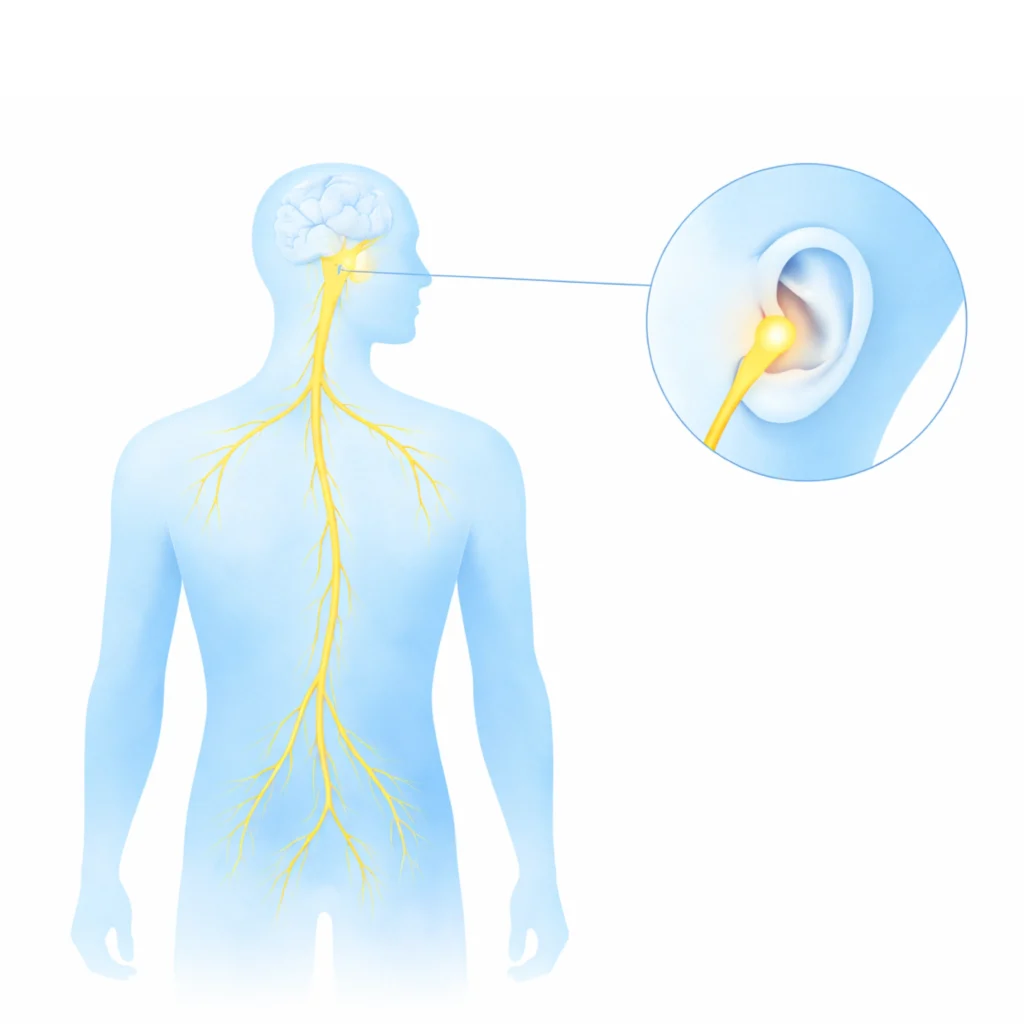
The vagus nerve controls parasympathetic activation.
This nerve runs from your brain through your body, signaling your heart, lungs, and digestive system to relax and recover.
When the vagal tone is weak, your parasympathetic system can’t do its job. Your HRV stays low and your body stays stuck in stress mode.
The solution isn’t just managing symptoms, it’s strengthening the system itself.
What the Research Shows: Vagus Nerve Stimulation and HRV
Researchers have been studying how stimulating the vagus nerve affects autonomic function. The evidence is compelling.
In randomized, placebo-controlled crossover studies, auricular vagus nerve stimulation (targeting the vagus nerve through the ear) has shown measurable effects on HRV.
Here’s what the research demonstrates:
The Setup
Studies compared active stimulation at the tragus (the small cartilage projection in front of the ear canal) with sham stimulation at the earlobe. Participants underwent 5-minute baseline periods, 5-minute stimulation periods, and 5-minute recovery periods, with continuous ECG monitoring to measure HRV changes.
The Results
Active tragus stimulation significantly increased multiple HRV metrics associated with parasympathetic activity:
- High-frequency (HF) HRV increased compared to placebo stimulation
- RMSSD, pRR50, and SDRR improved across the board
- The LF/HF ratio decreased, indicating a shift toward parasympathetic predominance
- Effects persisted into the recovery period, even after stimulation ended
The high-frequency component of HRV (0.15–0.40 Hz) is specifically linked to parasympathetic modulation. When HF HRV increases, it indicates stronger vagal influence on heart rate regulation.
In a controlled experiment in healthy adults, taVNS (tragus) increased several HRV indices compared with sham, with some effects persisting briefly into recovery. Symptom outcomes require separate studies.
Why This Matters
This isn’t a subtle effect. It’s measurable on the same devices you already use: Apple Watch, Oura Ring, WHOOP, or any ECG-based monitor.
The reason it works: auricular vagus nerve stimulation directly activates pathways in your parasympathetic nervous system. It signals your body to shift from “fight-or-flight” into “rest-and-digest.” With consistent use, this strengthens your vagal tone: the baseline activity of your vagus nerve.
Stronger vagal tone means:
- Your body recovers faster after stress
- Your HRV trends upward consistently
- You feel calmer without forcing it
- Sleep becomes more restorative
This approach has been tested in over 60+ scientific studies conducted in collaboration with elite institutions like Stanford, Yale, University of Chicago and UCLA.
It’s not experimental, it’s a scientifically validated method for supporting nervous system regulation.

Other Evidence-Based Methods to Improve HRV
Vagus nerve stimulation is the most direct intervention. But other approaches support HRV improvement when used consistently:
1. Prioritize Sleep Quality
Sleep duration and continuity are strongly linked to autonomic recovery. Sleep deprivation commonly reduces HRV, though the magnitude varies. Your nervous system recovers during deep sleep, especially REM and slow-wave stages.
What helps:
- Consistent sleep schedule (same bedtime/wake time daily)
- Cool, dark sleeping environment
- Limit screens 1-2 hours before bed
- Avoid alcohol close to bedtime (it suppresses REM sleep)
Aim for 7-9 hours per night. Track your HRV trends, you’ll see the impact of sleep quality immediately.
2. Manage Training Load
Intense exercise temporarily lowers HRV as your body recovers. This is normal. But chronic overtraining keeps HRV suppressed.
What helps:
- Balance hard training days with active recovery
- Monitor your HRV trends: if it stays low for days, rest longer
- Avoid high-intensity workouts when HRV is already low
- Prioritize recovery: stretching, mobility, low-intensity movement
If you’re training hard, your nervous system needs support to keep up with the stress load.
3. Reduce Chronic Stress
Easier said than done. But chronic stress keeps your sympathetic system activated, which directly suppresses HRV.
What helps:
- Breathwork: slow, diaphragmatic breathing (4-6 breaths per minute activates the parasympathetic system)
- Time in nature (proven to lower cortisol and improve HRV)
- Mindfulness or meditation (even 10 minutes daily helps)
- Limit stimulants: excessive caffeine keeps your nervous system wired
Stress management isn’t optional if you want lasting HRV improvement.
4. Limit Alcohol
Alcohol can dose-dependently reduce nocturnal recovery/parasympathetic activity, especially in the first hours of sleep; effects vary by dose and individual factors.
If you drink regularly, try reducing or eliminating alcohol for 2-3 weeks. Track your HRV. The difference is often dramatic.
5. Support Your Vagus Nerve Naturally
Some lifestyle practices gently stimulate vagal tone:
- Cold exposure (cold showers, ice baths)
- Humming or singing (vibrates the vagus nerve)
- Gargling water (activates throat muscles connected to the vagus)
These methods help. But they’re mild compared to direct vagus nerve stimulation, which delivers consistent, measurable activation.
The Fastest, Most Effective Approach: Nurosym
If you’re serious about improving HRV, there’s a direct path: strengthen your vagus nerve.
Nurosym is a wearable device that uses Auricular Vagal Neuromodulation Therapy (AVNT™): a scientifically validated method that stimulates the vagus nerve through the ear.
It’s the only certified wearable device designed specifically for this purpose. No surgery. Just gentle electrical signals delivered to the auricular branch of your vagus nerve.

Why Nurosym Works
Nurosym targets the root cause of low HRV: weak parasympathetic activation.
The device sends precisely calibrated signals to your vagus nerve. These signals activate your “rest-and-digest” system, training your nervous system to shift out of stress mode more easily.
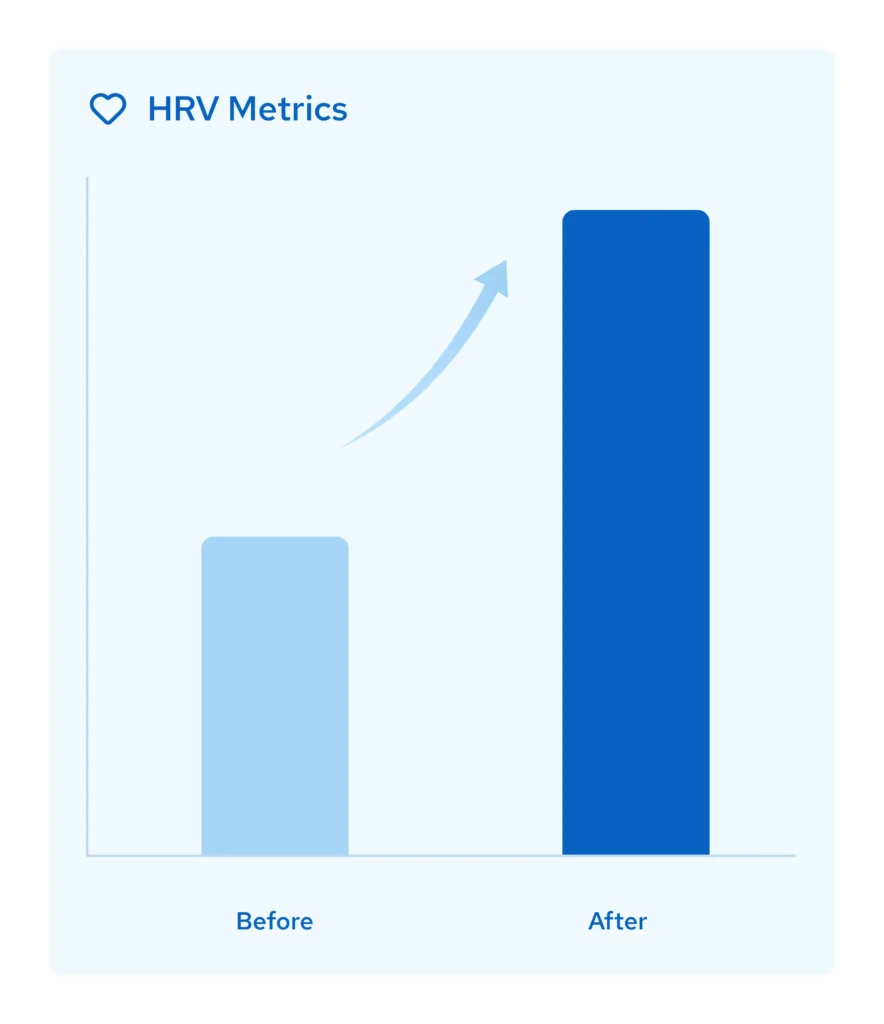
Over time, this strengthens your vagal tone. Your baseline HRV improves. Your body becomes more resilient.

The Science Behind It
Nurosym’s technology (AVNT™) has been tested in over 60 scientific studies, conducted in collaboration with institutions like Yale, Stanford or UCLA.
Results from studies include:
- 35% reduction in symptoms of anxious thoughts
- 48% reduction in fatigue and increase in energy
- 31% improvement in sleep scores
- 61% improvement in brain fog, gastrointestinal function and pain
- 45% improvement in depression score and improved mood
This isn’t a wellness gadget making broad claims. It’s a safe wearable device with FDA-reviewed safety standards (US) and CE certification.
How It Compares to Other Methods
Method | HRV Impact | Time to Results | Sustainability |
Vagus Nerve Stimulation (Nurosym) | Significant increase | 2-4 weeks | High: direct nervous system training |
Improved sleep | Moderate | Weeks | Moderate: requires perfect consistency |
Stress management (breathwork, meditation) | Mild | Months | Moderate: requires daily practice |
Cold exposure | Mild | Immediate (temporary) | Low: uncomfortable, hard to sustain |
Reduced alcohol | Moderate | Days | High: if maintained |

Nurosym addresses the system directly. You’re not trying to manage symptoms. You’re training your nervous system to regulate itself.
What Using Nurosym Looks Like
Nurosym is simple to use:
- Clip the device onto your ear (specifically the tragus, where the vagus nerve is accessible)
- Use it for 30-60 minutes daily: while working, reading, or relaxing
- Track your HRV on your Apple Watch, Oura Ring, or other device

Most users notice measurable HRV improvements within a few weeks. Some feel subjective changes sooner: better sleep, easier stress recovery, or more consistent energy.
The device integrates into your routine and you don’t need to learn a technique. You don’t need to change your schedule, just wear it whenever you want and wherever you go.
Why Nurosym Is the Obvious Choice
If you’ve been tracking your HRV, you already understand what’s at stake. You know low HRV isn’t just a number, it’s a signal that your body is struggling to recover.
You’ve probably tried the basics: more sleep, less stress, better training.
They help.
But they’re not enough if your nervous system is stuck.
Here’s why Nurosym is different:
Backed by Real Science & Results
- Over 4 million user sessions completed.
- Tested at elite institutions like Yale, UCLA, Stanford, University of Chicago Medicine and many other leading research institutions.
- Recommended by 1,000+ licensed healthcare professionals - This isn't a trend, it's validated medical technology.
- Efficacy confirmed in multiple peer-reviewed Randomised Placebo Controlles Studies.
Measurable Results
You can track your HRV before and after. Most users see improvements on their wearable devices within weeks. The effect is measurable, not subjective.
Safe and Non-Invasive
Nurosym has been designated by FDA as non-significant risk in multiple studies for safety (US standards) and CE-certified as a non-invasive neuromodulation device. It requires no surgery and has been proven with no serious side effects in studies reported up to date. Just gentle electrical signals that activate your parasympathetic system.

Easy to Use
Clip it on. Use it daily. That’s it.
No need for complicated techniques, time-consuming routines.
It is designed to fit into your life as easily as wearing headphones.
What You Can Expect
Within the first few weeks of using Nurosym daily, most users report:
- Measurable HRV increases visible on their tracking devices
- Easier recovery after stressful events or workouts
- Improved sleep depth and waking up more refreshed
- Reduced feelings of being "stuck" in stress or anxious thoughts
- More consistent energy throughout the day
The longer you use it, the stronger your vagal tone becomes. Think of it as training your nervous system: each session builds resilience.
One user described it this way:
“I absolutely love this device. It works perfectly and I haven’t had any problems so far. I highly recommend it.“
Another said:
“Overall, it’s something I wouldn’t want to be separated from. It’s my daily companion, it keeps me on the right track. And I imagine I’ll continue to use it for the rest of my life.”
These aren’t outliers. They’re typical of what happens when you give your nervous system the support it needs to improve your HRV.
Start Today
If you’ve been searching for how to improve your HRV, you already know the stakes. You know that low HRV isn’t just a number, it’s your body telling you it’s struggling.
You can keep managing symptoms with better habits. Or you can address the system directly.
Nurosym gives you a way to train your nervous system, strengthen your vagal tone, and see measurable results within weeks.
The science is clear.
The results are trackable.
And the solution is straightforward.

Final Thoughts: Your Nervous System Is Trainable
Heart rate variability isn’t static.
It’s not genetic.
It responds to how you support your nervous system.
Most people try to manage HRV indirectly: through sleep, stress management, or lifestyle changes. These help, but they’re not enough if your vagus nerve isn’t functioning properly.
Nurosym addresses the system directly: it trains your parasympathetic response. It strengthens the vagus nerve. And it gives you measurable results you can track in real time.
If you’re serious about improving your HRV, this is the most effective, science-backed approach available.
Your body is already trying to recover. Now you can give it the support it needs.
REFERENCES:
- de Brito, J. N., et al. (2020). The effect of green walking on heart rate variability: A pilot crossover study. Environmental Research, 185, 109408. https://doi.org/10.1016/j.envres.2020.109408
- Geng, Y., et al. (2022). Transcutaneous auricular vagus nerve stimulation modulates autonomic activity… PLOS ONE, 17(2), e0263833. https://doi.org/10.1371/journal.pone.0263833
- Gitler, A., et al. (2025). Harnessing non-invasive vagal neuromodulation: HRV… https://doi.org/10.3892/mi.2025.236
- Laborde, S., Mosley, E., & Thayer, J. F. (2017). Heart rate variability and cardiac vagal tone in psychophysiological research: Recommendations… Biological Psychology, 130, 1–??. https://doi.org/10.1016/j.biopsycho.2017.01.009
- Mizumoto, T., et al. (2025). Physiological adjustment effects of viewing natural environments… Scientific Reports. https://doi.org/10.1038/s41598-025-00681-4
- Muñoz, M. L., et al. (2018). [HRV genetic architecture paper]. Frontiers in Cardiovascular Medicine. https://doi.org/10.3389/fcvm.2018.00054
- Pietilä, J., et al. (2018). Acute effect of alcohol intake on cardiovascular autonomic regulation during the first hours of sleep… JMIR Mental Health, 5(1), e23. https://doi.org/10.2196/mental.9519
- Pop, G. N., et al. (2021). Assessment of the impact of alcohol consumption patterns on heart rate variability… Medicina, 57(9), 956. https://doi.org/10.3390/medicina57090956
- Sato, M., et al. (2025). Effects of sleep deprivation on autonomic function: A systematic review and meta-analysis. Frontiers in Neuroscience. https://doi.org/10.3389/fnins.2025.1560531
- Schumann, A., et al. (2022). [Slow-paced breathing systematic review/meta-analysis]. Neuroscience & Biobehavioral Reviews. https://doi.org/10.1016/j.neubiorev.2022.104711
- Shaffer, F., & Ginsberg, J. P. (2017). An overview of heart rate variability metrics and norms. Frontiers in Public Health, 5, 258. https://doi.org/10.3389/fpubh.2017.00258
- Shao, R., et al. (2024). The effect of slow-paced breathing on cardiovascular and psychological outcomes… Mindfulness. https://doi.org/10.1007/s12671-023-02294-2
- Tegegne, B. S., et al. (2020). [HRV heritability/genetics paper]. BMC Medical Genetics. https://doi.org/10.1186/s12881-020-01181-2
The article does not in any way constitute as medical advice. Please seek consultation with a licensed medical professional before starting any treatment. This website may receive commissions from the links or products mentioned in this article.
Share via:


