A comprehensive review of how VNS devices restore autonomic function by addressing nervous system dysregulation—with expert rankings of the top 4 certified options.

Postural Orthostatic Tachycardia Syndrome (POTS) is estimated to affect between 1 and 3 million people in the United States, causing debilitating symptoms when transitioning from lying to standing. Unlike simple dehydration or deconditioning, Postural Heart Rate Abnormalities reflects a fundamental dysfunction of the autonomic nervous system dysfunction, disrupting cardiovascular regulation, blood flow distribution, and cellular energy metabolism.
Recent neuroscience research suggests that vagus nerve dysfunction may be an important contributing mechanism in a subset of Postural Heart Rate Abnormalities individuals, alongside hypovolemia, peripheral neuropathy, hyperadrenergic states, and autoimmune processes. When this principal parasympathetic nerve demonstrates reduced activity, the body may lose some capacity to modulate heart rate appropriately, maintain cerebral perfusion, and regulate peripheral vascular tone.
This guide examines the relationship between vagus nerve function and Postural Heart Rate Abnormalities symptomatology and evaluates the leading vagus nerve stimulation (VNS) devices that may help restore autonomic balance and functional capacity.
Symptoms of Postural Heart Rate Abnormalities
Postural Heart Rate Abnormalities are characterised by an excessive increase in heart rate (≥30 bpm in adults, ≥40 bpm in adolescents) within 10 minutes of standing, without orthostatic hypotension. Common manifestations include:
Cardiovascular symptoms:
- Heart rate elevation exceeding 120 bpm upon standing
- Palpitations or sensation of rapid, forceful heartbeat
- Chest discomfort or pressure
- Peripheral vascular dysregulation (venous pooling, cold extremities, colour changes)
- Presyncope (lightheadedness, near-fainting episodes)
- Syncope (actual loss of consciousness)
Cerebrovascular symptoms:
- Cognitive impairment ("brain fog"), particularly when upright
- Visual disturbances (tunnel vision, blurred vision, visual snow)
- Difficulty with concentration and information processing while upright
- Memory consolidation problems
- Headaches (often orthostatic in nature)
Autonomic dysregulation:
- Temperature dysregulation (heat intolerance, inappropriate sweating)
- Gastrointestinal dysmotility (nausea, early satiety, constipation, diarrhoea)
- Urinary frequency or urgency
- Tremulousness or internal tremor sensation
- Exercise intolerance with prolonged recovery periods
Systemic symptoms:
- Profound fatigue unrelated to exertion level
- Sleep architecture disruption
- Anxious thoughts (often secondary to physical symptoms)
- Muscle weakness or pain
- Post-exertional malaise lasting 24-48 hours
The functional impact extends beyond symptomatology: inability to maintain employment, educational disruption, social isolation, loss of independence, and significant reduction in quality of life metrics.

Postural Heart Rate Abnormalities Self-Assessment
Evaluate the symptoms you experience with regularity:
Cardiovascular Function
- Heart rate increases ≥30 bpm within 10 minutes of standing
- Palpitations or rapid heartbeat when upright
- Lightheadedness or near-fainting upon standing
- Cold hands and feet despite adequate ambient temperature
- Chest discomfort when upright
Cerebrovascular Function
- Brain fog or cognitive slowing when standing
- Visual disturbances (dimming, tunnel vision, floaters)
- Difficulty maintaining concentration in the upright position
- Headaches that improve when lying down
- Memory problems affecting daily function
Postural Tolerance
- Must sit or lie down frequently throughout the day
- Cannot stand for more than 10-15 minutes
- Symptoms worsen in warm environments
- Morning symptoms are particularly severe
- Shower or bathing triggers symptom exacerbation
Autonomic Symptoms
- Gastrointestinal problems (nausea, bloating, altered motility)
- Temperature regulation difficulties
- Excessive or insufficient sweating
- Tremor or shakiness
- Sleep disruption despite fatigue
Functional Capacity
- Unable to work or attend school full-time
- Exercise causes a multi-day symptom flare
- Must plan activities around symptom management
- Significant lifestyle modifications required
- Normal blood pressure readings despite symptoms
Diagnostic History
- Symptoms began after a viral illness, pregnancy, surgery, or trauma
- Tilt table test confirmed excessive heart rate increase
- The cardiologist ruled out primary cardiac pathology
- Standard autonomic testing shows abnormalities
- Conventional interventions provide incomplete relief
If you identify with multiple features across the cardiovascular, postural tolerance, and autonomic categories, Postural Heart Rate Abnormalities may be a consideration and warrant formal evaluation by a clinician experienced in autonomic disorders.
In some individuals, impaired vagal tone and parasympathetic withdrawal may contribute to symptom severity, making therapies that support autonomic regulation a potential adjunct, under medical guidance.
Vagus nerve stimulation may warrant discussion with your healthcare provider as an adjunctive approach.
The Vagus Nerve Connection
What Is the Vagus Nerve?
The vagus nerve (cranial nerve X) is the longest and most complex nerve of the autonomic nervous system, originating in the medulla oblongata and projecting through the neck to innervate the heart, lungs, and gastrointestinal tract. It mediates critical homeostatic functions:
- Cardiovascular regulation (chronotropic and dromotropic modulation)
- Respiratory pattern generation
- Gastrointestinal motility and secretion
- Inflammatory reflex pathway (cholinergic anti-inflammatory pathway)
- Baroreceptor reflex integration
- Metabolic regulation
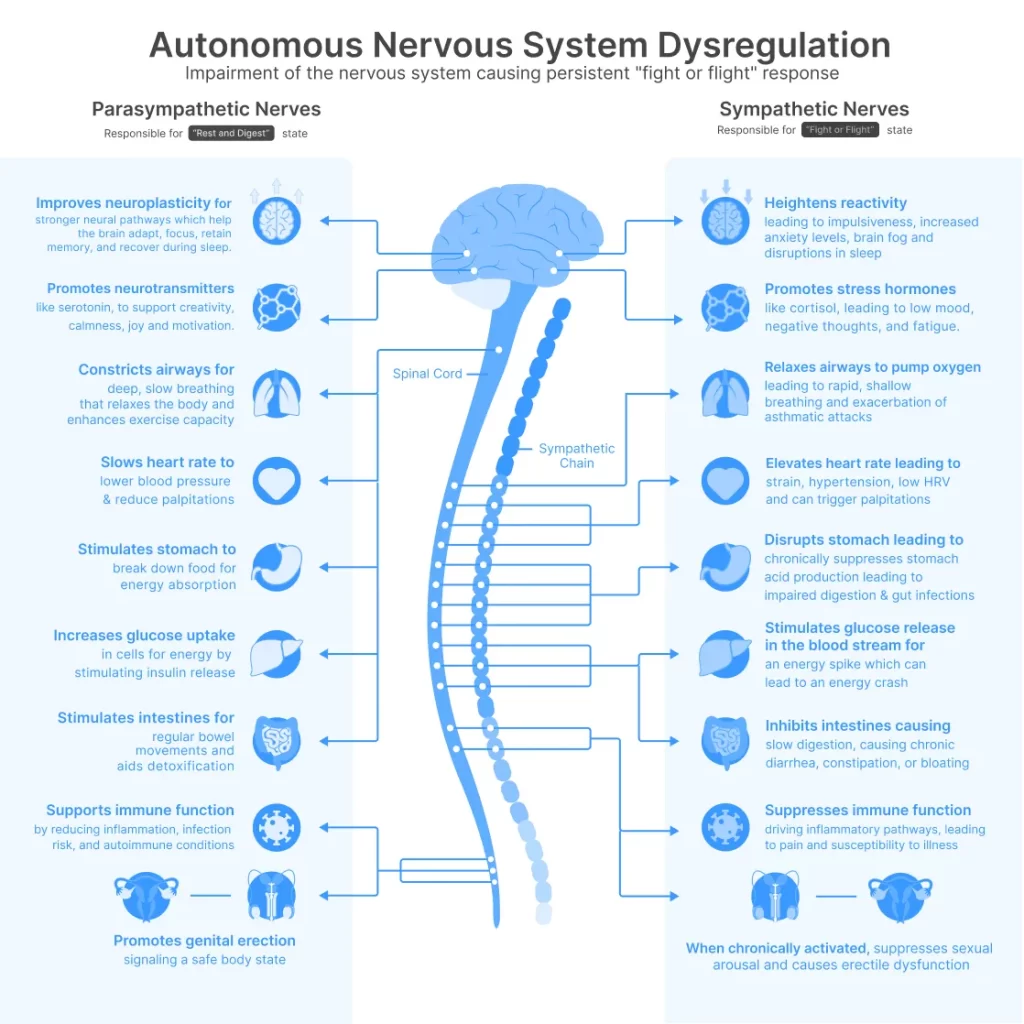
The Two-Mode System
Your autonomic nervous system operates through two complementary divisions:
- Sympathetic (thoracolumbar outflow): Increases heart rate, elevates blood pressure, mobilises glucose, redistributes blood flow to skeletal muscle—activated during stress or perceived threat.
- Parasympathetic (vagal outflow): Controlled predominantly by the vagus nerve, reduces heart rate, promotes digestion, facilitates recovery, supports cellular restoration and repair mechanisms.
Healthy autonomic function requires a dynamic balance between these systems, with rapid shifts based on postural demands, environmental context, and metabolic requirements. However, infection, autoimmune activation, or sustained stress can impair vagal tone, creating sympathetic predominance.
How Vagus Nerve Dysfunction Causes Postural Heart Rate Abnormalities
When your vagus nerve demonstrates reduced activity (low vagal tone):
- Cardiovascular dysregulation: Loss of parasympathetic counterbalance to sympathetic activation causes excessive heart rate acceleration upon standing. Without appropriate vagal braking, a rapid heartbeat becomes the primary compensatory mechanism for maintaining cardiac output and cerebral perfusion.
- Impaired baroreceptor sensitivity: The vagus nerve transmits arterial baroreceptor signals to the brainstem cardiovascular centres. Dysfunction impairs this feedback loop, preventing appropriate blood pressure and heart rate adjustments during postural changes.
- Peripheral vascular abnormalities: Reduced vagal activity contributes to inadequate vasoconstriction in the lower extremities, allowing venous pooling. As much as 500–800 mL of blood may pool in the lower extremities and splanchnic circulation upon standing, reducing venous return and triggering compensatory rapid heartbeat.
- Reduced heart rate variability (HRV): HRV serves as a validated biomarker of vagal tone. Postural Heart Rate Abnormalities individuals consistently demonstrate markedly reduced HRV, indicating parasympathetic withdrawal and reduced capacity for cardiovascular adaptation.
- Chronic sympathetic activation: Compensatory sympathetic overdrive maintains elevated norepinephrine levels (often 2-3x normal when standing), causing tremor, anxious thoughts, sweating, and progressive receptor desensitisation—worsening symptoms over time.
- Inflammatory dysregulation: The vagus nerve controls the cholinergic anti-inflammatory pathway. Dysfunction permits chronic low-grade inflammation, which directly impairs endothelial function, mitochondrial efficiency, and cellular energy production—contributing to fatigue and exercise intolerance.
It is important to note that Postural Heart Rate Abnormalities is a heterogeneous syndrome rather than a single disease entity. Vagus nerve dysfunction does not account for all cases. Some individuals exhibit predominant hypovolemia, others neuropathic or hyperadrenergic features, and many demonstrate overlapping mechanisms. Vagal impairment appears most relevant in individuals with reduced heart rate variability, autoimmune markers, or post-viral onset.

The Scientific Evidence
Published research establishes clear relationships between vagus nerve dysfunction and Postural Heart Rate Abnormalities pathophysiology:
- Autonomic dysfunction profile: Studies document that Postural Heart Rate Abnormalities individuals exhibit distinct autonomic abnormalities consistent with impaired vagal and sympathetic cardiovascular control, including decreased vagal baroreflex sensitivity and impaired sympathetic responsiveness. Heart rate variability parameters—validated biomarkers of vagal tone—are markedly reduced compared to healthy controls.
- Autoimmune mechanisms: Growing evidence indicates Postural Heart Rate Abnormalities may represent an autoimmune disorder. Research demonstrates increased expression of autoantibodies against adrenergic and muscarinic acetylcholine receptors in Postural Heart Rate Abnormalities individuals. Alpha-1 adrenergic receptor (α-1 AR) autoantibodies are significantly elevated in most individuals with Postural Heart Rate Abnormalities, with a subset of individuals (approximately 20–30% in some cohorts) showing elevated α1-AR and α2-AR antibodies. These adrenergic receptor autoantibodies correlate significantly with orthostatic intolerance severity—a cardinal Postural Heart Rate Abnormalities feature.
- Scientific trial evidence for vagus nerve stimulation: A randomised, double-blind, placebo-controlled scientific trial conducted at the University of Oklahoma Health Sciences Center (led by Associate Professor Stavros Stavrakis) demonstrated scientifically meaningful improvements in orthostatic rapid heartbeat associated with transcutaneous vagus nerve stimulation for Postural Heart Rate Abnormalities:
- Study design: 26 participants (active n=12, placebo n=14) received one hour daily stimulation for 2 months using auricular vagus nerve stimulation technology
- Primary outcome: Postural rapid heartbeat was significantly reduced in the active group versus the placebo. Postural heart rate increase was 18±10 bpm in the therapy group compared to 32±14 bpm in the placebo (p=0.016)—representing a scientifically meaningful 14 bpm difference.
- Mechanistic findings: Anti-autonomic autoantibodies were significantly lower in the therapy group after 2 months compared to placebo, providing mechanistic insight into Postural Heart Rate Abnormalities pathophysiology
- Safety profile: No device-related adverse events were reported; all subjects demonstrated excellent adherence to the protocol
- Evidence classification: This represents Level IB evidence according to the Center for Evidence-Based Medicine recommendations—providing strong support for scientific application
- Post-viral Postural Heart Rate Abnormalities connection: Post-viral syndromes, including Postural Heart Rate Abnormalities following SARS-CoV-2 infection, demonstrate marked vagal impairment and elevated inflammatory markers that are normally regulated by vagal anti-inflammatory pathways. Studies indicate that a small but scientifically significant proportion of individuals recovering from SARS-CoV-2 infection develop Postural Heart Rate Abnormalities or Postural Heart Rate Abnormalities-like autonomic dysfunction, particularly following moderate to severe illness.
- The mechanistic conclusion: Restoring vagus nerve function through targeted stimulation addresses the underlying autonomic and immunological pathophysiology of Postural Heart Rate Abnormalities—including both parasympathetic withdrawal and autoantibody-mediated dysfunction—rather than merely suppressing symptoms.
VNS Devices as a Solution: How They Work
The Technology Revolution
Until recently, vagus nerve stimulation required invasive surgical procedures—implanting electrodes directly on the nerve through operations that carried surgical risks, recovery time, and permanent device placement. This confined VNS therapy primarily to therapy-resistant cases of depressive states where the benefits justified surgical intervention.
Today’s breakthrough changes everything.
Modern transcutaneous vagus nerve stimulation (tVNS) delivers the same therapeutic electrical impulses to the vagus nerve—facilitating neuroplastic adaptation and restoration of appropriate tone—but completely non-invasively through the skin. No surgery. No implantation. No recovery period.
These advanced devices achieve remarkable effectiveness with an exceptional safety profile, operating through precisely positioned electrodes at two accessible locations:
- Cervically (neck): Targeting the cervical branch of the vagus nerve near the carotid artery, where the nerve courses superficially beneath the skin
- Auricular (ear): Targeting the auricular branch of the vagus nerve innervating the tragus and cymba conchae—the only place cranial nerves reach the body's surface
This represents a fundamental shift: vagus nerve stimulation therapy that was once confined to operating rooms is now available for daily home use, with scientific-grade precision and zero surgical risk.
Mechanism of Action
When precisely calibrated electrical impulses reach the vagus nerve, they initiate a cascade of neurophysiological responses:
- Neurotransmitter modulation: Stimulation triggers release of acetylcholine at parasympathetic terminals, directly counteracting sympathetic predominance and activating cholinergic anti-inflammatory pathways
- Brainstem nucleus activation: Afferent vagal signals project to the nucleus tractus solitarius, which integrates autonomic regulatory information and modulates cardiovascular control centres in the medulla
- Autonomic rebalancing: Consistent stimulation protocols facilitate a shift from sympathetic dominance toward parasympathetic restoration, improving heart rate variability and baroreflex sensitivity
- Neuroplasticity enhancement: VNS promotes synaptic reorganisation in central autonomic networks, potentially restoring normal cardiovascular regulatory capacity
- Inflammatory suppression: Vagal stimulation activates the cholinergic anti-inflammatory pathway, reducing pro-inflammatory cytokine production (TNF-α, IL-1β, IL-6) that contributes to endothelial dysfunction and symptom perpetuation
Clinical Parameters
Research-validated VNS protocols typically employ:
- Session duration: 30-60 minutes daily (allowing for sustained neurophysiological effects)
- Intensidad: Individualised to sensory threshold (perceptible but comfortable stimulation)
- Consistency: Daily application for a minimum of 8-12 weeks (neuroplastic changes require sustained intervention)
Expected Timeline
VNS promotes gradual nervous system adaptation rather than immediate symptom suppression:
- Week 1-2: Enhanced relaxation response during stimulation sessions, modest improvements in sleep architecture, possible mild reduction in resting heart rate
- Week 3-4: Noticeable improvements in orthostatic tolerance, reduced rapid heartbeat intensity, decreased presyncope frequency, improved cognitive function when upright
- Month 2-3: Sustained cardiovascular stability, increased standing tolerance, reduced symptom severity, measurable HRV improvements, decreased reliance on symptom management strategies
- Month 3+: Restored autonomic balance, functional capacity improvements, ability to resume previously limited activities, enhanced quality of life metrics
Safety Considerations
VNS using transcutaneous approaches is generally well-tolerated in scientific research. Potential transient responses may include:
- Mild tingling sensation at the stimulation site
- Temporary muscle tension in the neck region (cervical devices)
- Brief lightheadedness (typically resolves with protocol adjustment)
Important limitations: Not appropriate for individuals with cardiac pacemakers, recent acute cardiac events, pregnancy, or a history of vagotomy. Healthcare provider consultation is essential prior to initiating any VNS protocol.
Top 4 VNS Devices for Postural Heart Rate Abnormalities
#1: Nurosym
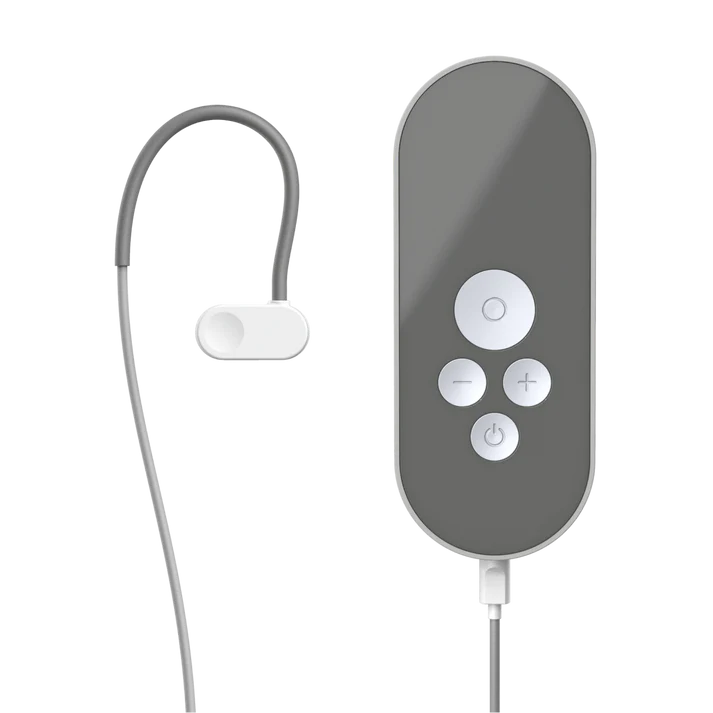
Price: 700 EUR Varies by region (€40 research subsidy available)
Type: Auricular (ear-worn)
Technology: AVNT™ by Parasym
Why #1:
- Most extensively validated: Supported by 50+ peer-reviewed publications from Harvard Medical School, UCLA, and leading research institutions worldwide.
- Demonstrated efficacy for autonomic dysfunction: Scientific studies document 61% improvement in vagal tone (HRV metrics), significant reduction in sympathetic overactivation, and improved cardiovascular regulation.
- Independent certification: CE-marked wearable device meeting rigorous safety and performance standards—third-party verified.
- Scientific adoption: Used by 1000+ healthcare professionals and researchers; integrated into institutional protocols; 4,000,000+ supervised stimulation sessions completed.
- Evidence-based parameters: Stimulation protocols derived from peer-reviewed research, not proprietary guesswork.
- Comprehensive support: 30-day evaluation period, scientific guidance resources, responsive technical support.
Ideal para: Individuals seeking the most scientifically validated device, particularly those with autonomic dysfunction (Postural Heart Rate Abnormalities, dysautonomia), post-viral syndromes, or those prioritising evidence over marketing claims.
#2: Truvaga Plus

Price: $544+ (device $499 + spray $45/year + potential subscription) Type: Cervical (neck handheld)
Technical note: Shares core technology with gammaCore, an FDA-cleared device for migraine/cluster headache (not Postural Heart Rate Abnormalities). Rapid parasympathetic effects. Straightforward protocol.
Considerations: Ongoing costs for conductive spray plus potential app subscription—verify pricing before purchase. Common adverse effects include muscle spasms, facial droop, lip pull, and headache. Not suitable for users with cardiac states, pacemakers, or recent heart issues. Mobile app connectivity problems reported.
Ideal para: Those preferring cervical stimulation with FDA-cleared technology lineage (for migraine, not Postural Heart Rate Abnormalities) who can tolerate potential facial muscle spasm adverse effects.
#3: Pulsetto

Price: $350-$371 (device $269 + gel $81-$102/year) Type: Cervical (hands-free collar)
Advantages: Hands-free wearable design. HSA/FSA eligible. 2-year warranty coverage.
Critical Limitations: No peer-reviewed scientific studies demonstrating efficacy for Postural Heart Rate Abnormalities—only company press releases and retail testimonials. Frequent fit problems create inadequate nerve contact, especially with smaller necks. Users consistently report minimal to no improvement in Postural Heart Rate Abnormalities symptoms compared to research-validated devices.
Not recommended for Postural Heart Rate Abnormalities: The $200-350 price difference seems attractive until you calculate the real cost: months of continued disability while using an unproven device. Lower-cost devices may appear attractive; however, the absence of scientific validation means their effectiveness for autonomic disorders like Postural Heart Rate Abnormalities remains uncertain.
#4: Sensate

Price: $299-$349 Type: Chest-worn vibrotactile device (not true VNS)
Advantages: Comfortable pebble design worn on the chest. Simple app interface with soundscapes. Lower price point. Can be used while performing other activities with a neck strap.
Critical distinction: Sensate does not directly stimulate the vagus nerve through electrical impulses like other devices in this comparison. Instead, it uses infrasonic vibrations and bone conduction placed on the chest—an indirect approach targeting general stress reduction rather than specific vagal nerve activation. While bone conduction at the ear has some research supporting vagal stimulation, Sensate’s chest placement lacks scientific substantiation for direct vagus nerve engagement. The mechanism is fundamentally different: actual VNS devices (like Nurosym, Truvaga, and Pulsetto) deliver calibrated electrical signals directly to accessible vagus nerve branches; Sensate delivers vibrations to your sternum, hoping for downstream effects.
For Postural Heart Rate Abnormalities individuals: This matters significantly. Postural Heart Rate Abnormalities require restoration of measurable autonomic function—improved heart rate variability, reduced orthostatic rapid heartbeat, enhanced baroreflex sensitivity. General relaxation devices may help with stress management, but do not address the underlying vagal dysfunction and autonomic dysregulation driving Postural Heart Rate Abnormalities symptoms. No scientific studies demonstrate Sensate’s efficacy for Postural Heart Rate Abnormalities or autonomic disorders—only company-funded studies showing general stress reduction in healthy volunteers.
Ideal para: Those seeking a general relaxation and stress management tool rather than targeted vagus nerve stimulation for autonomic dysfunction. Not recommended for individuals prioritising evidence-based Postural Heart Rate Abnormalities therapy.
*With a €70 research subsidy for qualifying participants
**Requires meticulous intensity management and protocol adherence
Conclusion: Nurosym offers the most comprehensive scientific validation, proven efficacy for autonomic dysfunction, including Postural Heart Rate Abnormalities, independent regulatory certification, and optimal balance of research foundation and practical application for those prioritising evidence-based outcomes.
Take Action
Postural Heart Rate Abnormalities related to vagus nerve dysfunction represent a symptom with emerging, adjunctive therapeutic approaches. Your autonomic nervous system possesses the capacity for neuroplastic adaptation and restoration of regulatory function.
With support from 50+ scientific studies, independent CE-marking certification, and 4,000,000+ documented stimulation sessions, Nurosym provides scientifically validated potential for restoring autonomic balance and functional capacity.
This information is provided for educational purposes. VNS devices are not intended to diagnose, treat, cure, or prevent any disease. Individuals with Postural Heart Rate Abnormalities should work with qualified healthcare providers to develop comprehensive management strategies. Always consult your physician before beginning any new intervention.
Fuentes
- Stavrakis S, Chakraborty P, Farhat K, Whyte S, Morris L, Zain, et al. Noninvasive Vagus Nerve Stimulation in Postural Tachycardia Syndrome. JACC: Clinical Electrophysiology. 2023 Nov 1;
- Wang Z, Zhu T, Li X, Lai X, Chen M. Tragus Nerve Stimulation Attenuates Postural Orthostatic Tachycardia Syndrome in Post COVID‐19 Infection. Clinical Cardiology. 2025 Feb 27;48(3).
- Stavrakis S, Cai X, Morris L, Whyte S, Karfonta B, Matlock HG, et al. LB-456640-4 NONINVASIVE VAGUS NERVE STIMULATION IN POSTURAL TACHYCARDIA SYNDROME: A RANDOMIZED CLINICAL TRIAL. Heart Rhythm. 2023 Jul 1;20(7):1090–0.
- Shiffer D, Rigo S, Minonzio M, Yarsuvat DT, Tobaldini E, Furlan L, et al. Short and long term effects of a two-week transcutaneous vagus nerve stimulation in hyperadrenergic postural orthostatic tachycardia syndrome: a proof-of-concept trial. European Journal of Internal Medicine [Internet]. 2025 Sep 27;106529. Available from: https://www.sciencedirect.com/science/article/abs/pii/S0953620525004078
Compartir a través de:

